Digital, self-guided CBT proven to be effective, if made accessible.
Most Australian insomniacs struggle to access timely and affordable CBT and instead rely on prescribed sleeping pills.
According to data from BEACH and the 2019 Sleep Health Foundation Insomnia Survey, only 1% of Australians with insomnia are referred to a psychologist for cognitive behavioural therapy, the recommended first line treatment, while 90% are managed with medication.
Now, new Australian research, published in Frontiers in Sleep, reports an interactive and digital insomnia-specific CBT program can lead to large, sustained improvements in insomnia, depression and fatigue for up to 16 weeks.
“It is vital that we develop and implement an effective evidence-based management approach for this condition,” said lead author Dr Alexander Sweetman (PhD), a research fellow from Flinders University, in a statement.
The study, including over 60 patients with moderate insomnia, examined the effectiveness of a free digital CBT program (Bedtime Window) involving five weekly sessions of up to 30 minutes each.
“The program includes algorithms that continuously assess for symptoms of sleepiness and alertness and provides tailored and interactive recommendations to treat insomnia without worsening levels of daytime sleepiness,” Dr Sweetman said in a statement.
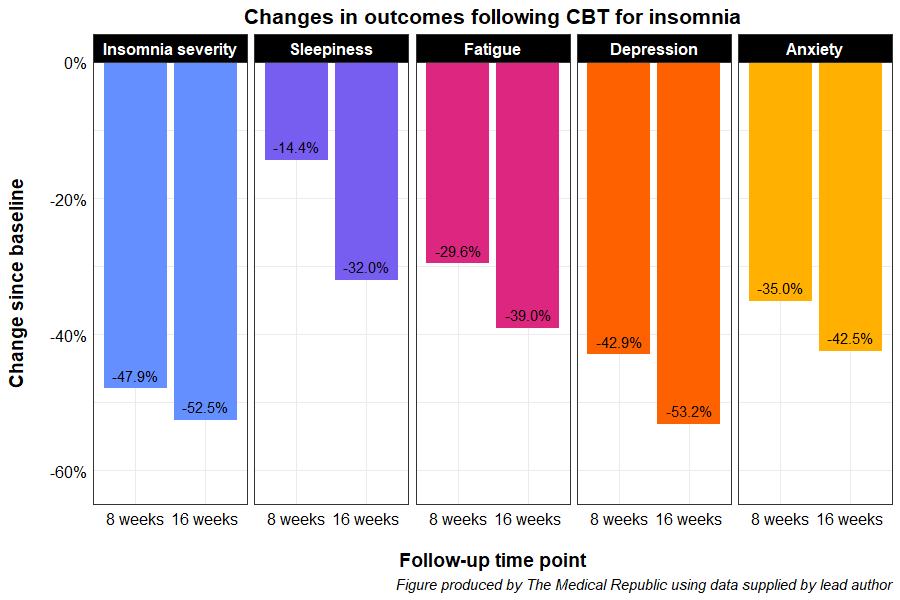
Participants reported significant reductions in insomnia severity, sleepiness, fatigue, depression and anxiety at the eight- and 16-week follow-ups compared to pre-CBT levels.
- There were no significant differences in outcomes between patients with only insomnia and those suspected to have insomnia and comorbid OSA.
“Those at high-risk of OSA benefited from this digital CBT program at least as much as those with insomnia alone… Suggesting that the program may be an effective, safe and scalable treatment for insomnia in people with suspected [comorbid insomnia and sleep apnoea],” the study authors wrote.
Related
A key limitation of the study was that only questionnaire data was used, rather than looking at potential changes to sleep patterns. Furthermore, patients with a previous diagnosis of OSA or any other comorbid sleep disorder were excluded from the study, and insomnia and sleep apnoea were self-reported rather than having been diagnosed with a sleep study – meaning the results may not generalise to these populations.
The researchers are providing free access to the digital CBT program via an ongoing GP referral study. Any Australian GP can sign up to access and refer patients for the freely available treatment as part of the trial.





