Medication history provides an important adjunct to imaging for diagnosing this case of non-traumatic shoulder pain.
History
This 76-year-old female presented with pain for a number of months and a recent exacerbation in her left shoulder. She experienced painful swelling, along with pain on overhead activity. She denied any traumatic event. There was a painful arc and objective supraspinatus and infraspinatus weakness on clinical examination.
Image findings
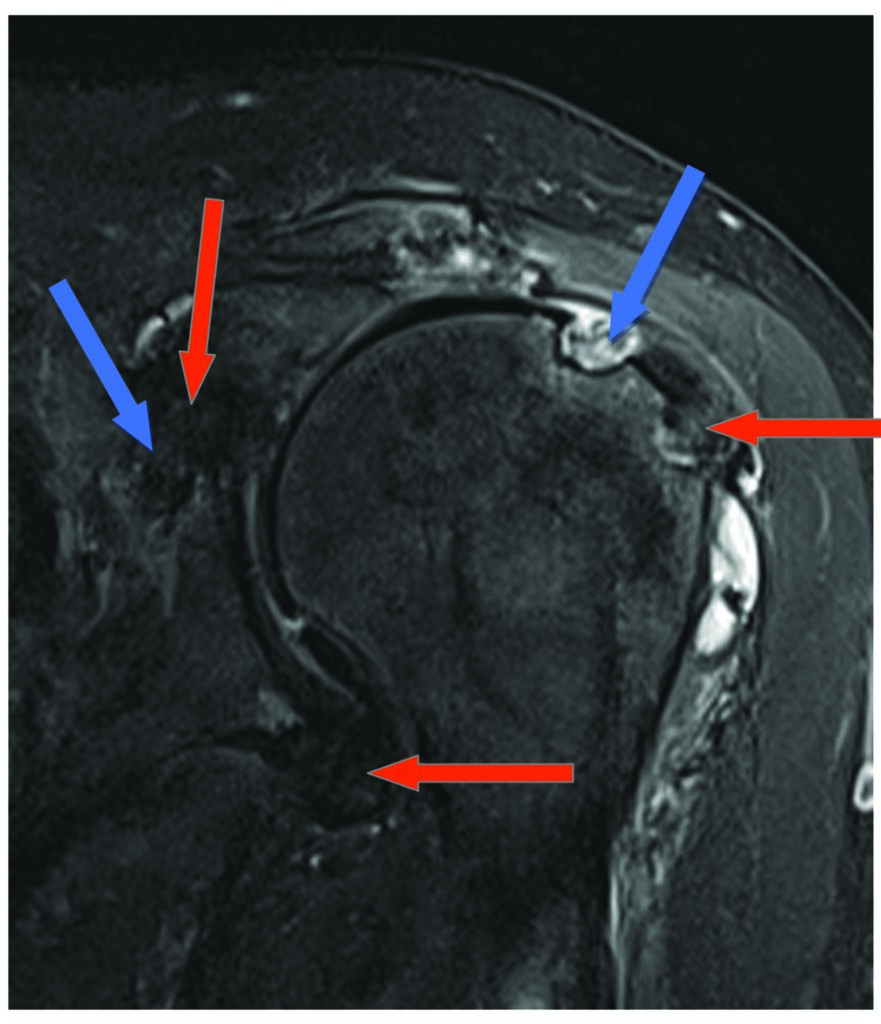
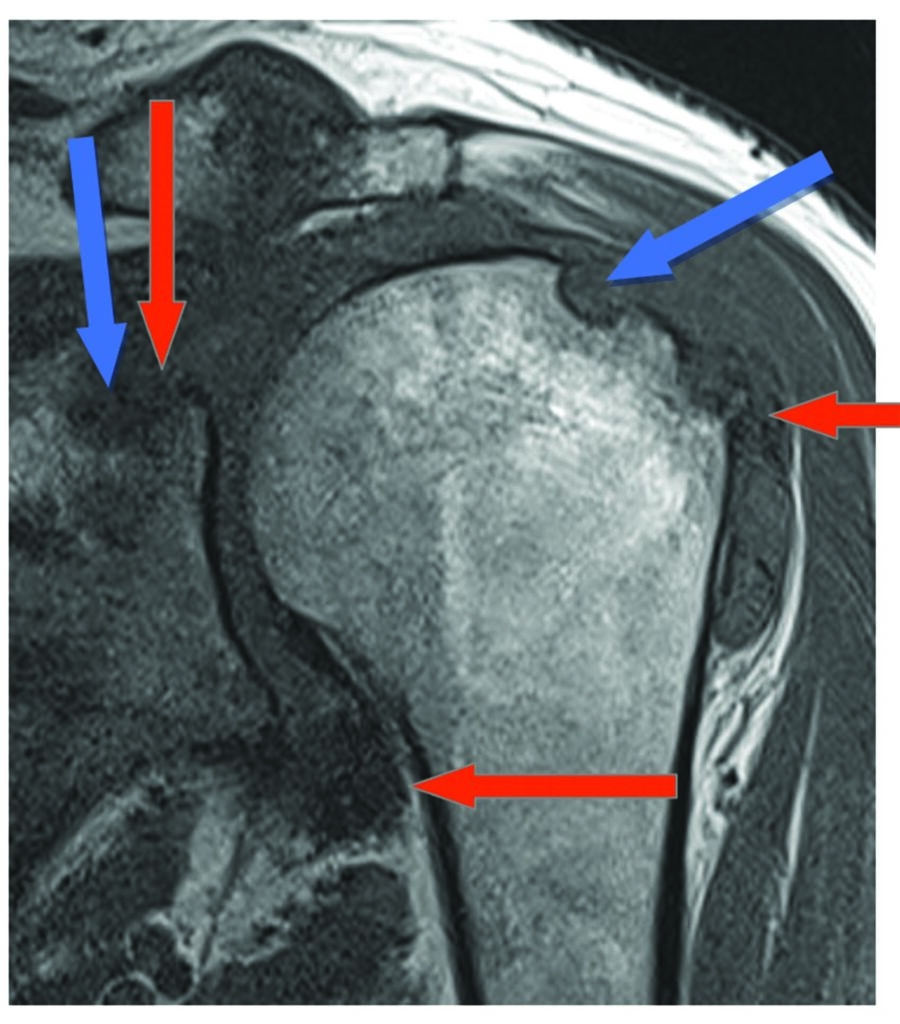
An initial X-ray was performed that demonstrated worrying ill-defined lucency involving the humeral head with cortical destruction, raising the possibility of a malignant infiltrative process. This warranted further investigation with a CT, which demonstrated lucent destructive lesions both in the superolateral humeral head and the glenoid (as well as at the under surface of the acromion).
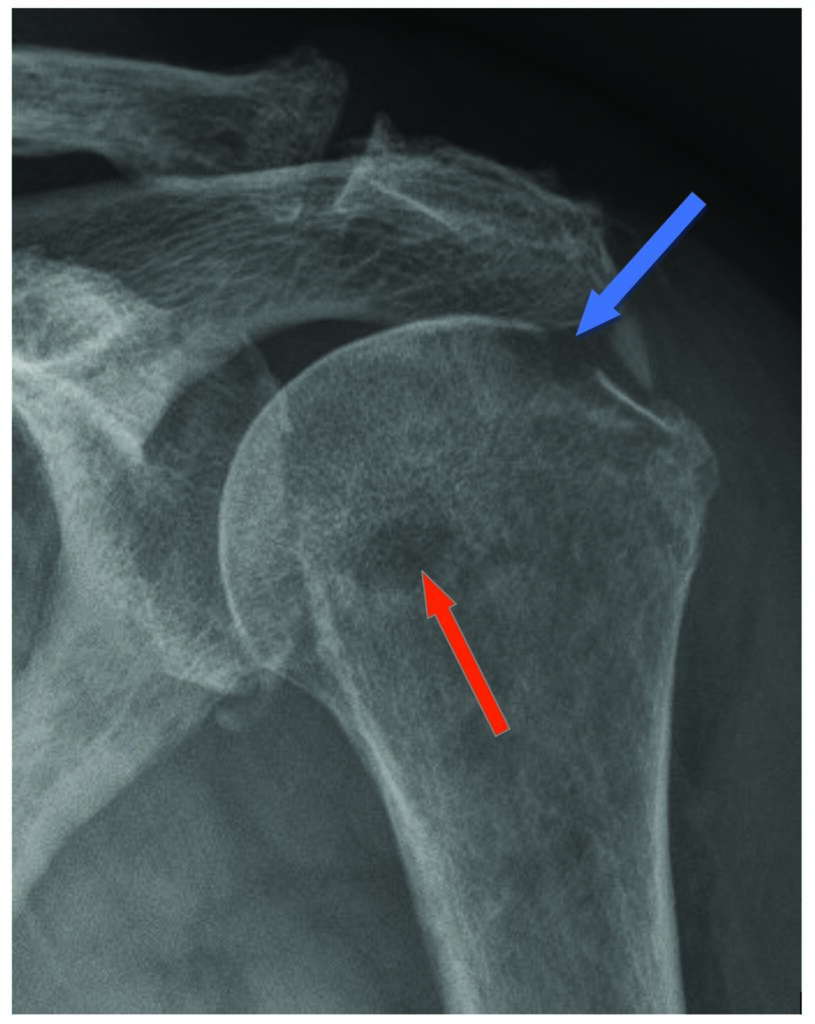
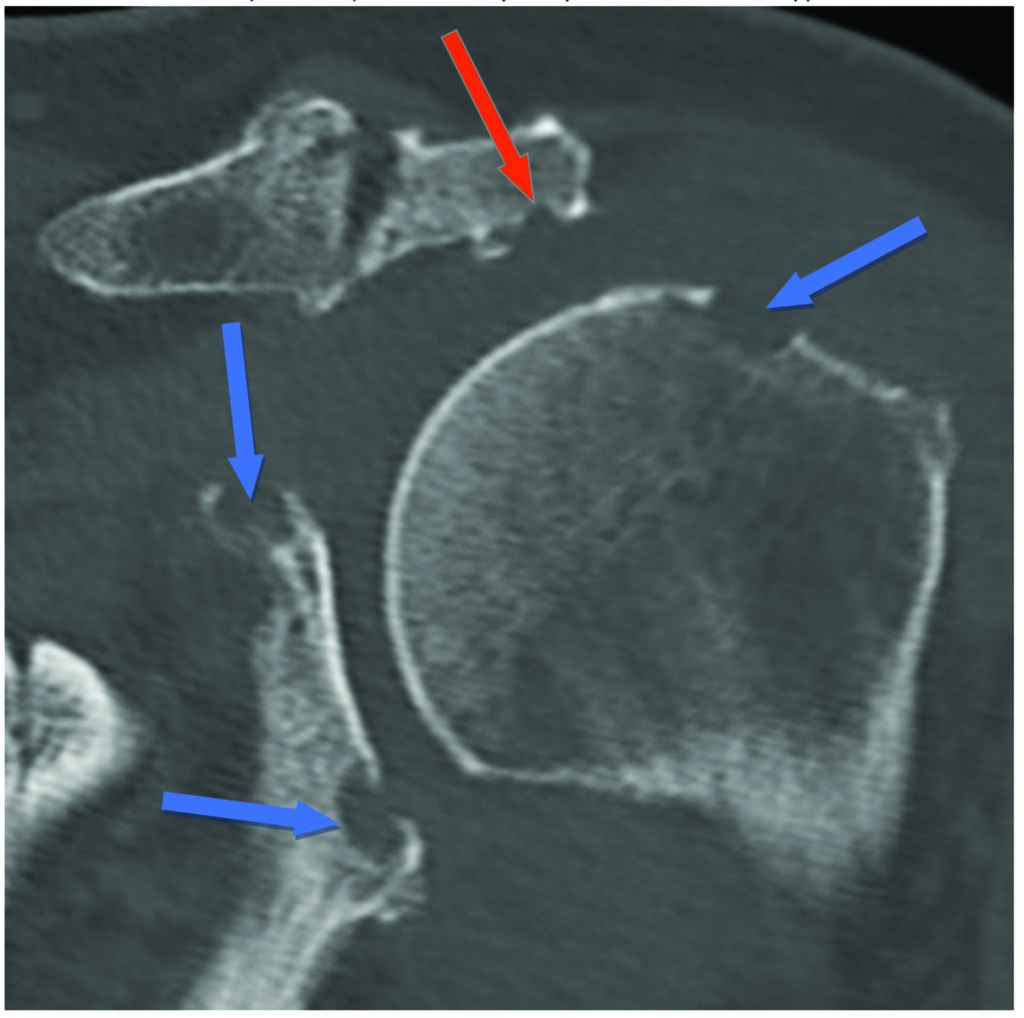
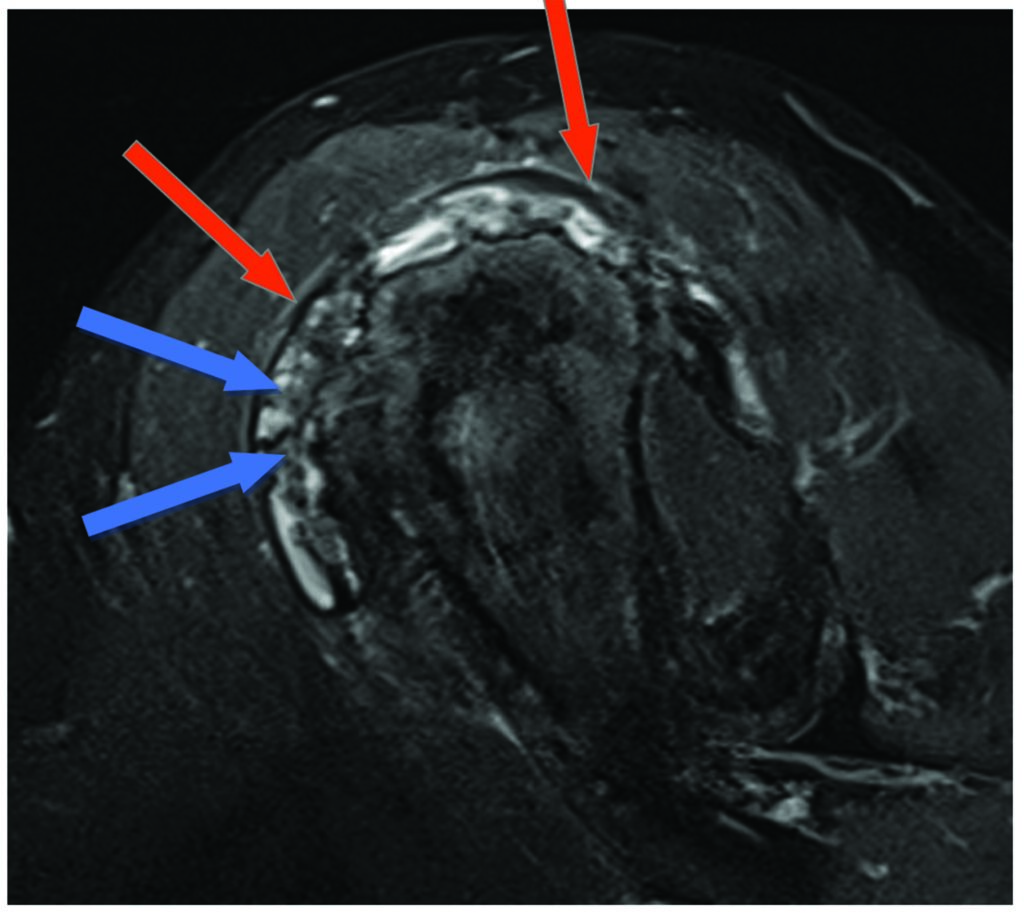
Initially this was thought to confirm a destructive aggressive process, but the imaging was reviewed. It was noted that these lucent lesions were at the periphery of the joint, and there was no destructive lesion within the marrow. The patient also had a history of anticoagulation due to a metallic mitral valve implanted 15 years prior.
Fortunately, this was compatible with MRI, which demonstrated marginal erosions accounting for the humeral and glenoid lucency on CT/Xray. There was little marrow oedema and no marrow infiltration or low-signal T1 in the marrow to suggest a malignant process. In addition, there was prominent low-signal synovial proliferative thickening diffusely throughout the glenohumeral joint – this low signal represents hemosiderin staining. A massive rotator cuff acute on chronic tear with muscle oedema and atrophy is also present.
Analysis
This case illustrates several important imaging tenets. The presence of bony changes on both sides of a joint, particularly at the joint margins, indicates a joint-centred pathology rather than a bone-centred pathology. The location of bony destruction at the joint margins, and the absence of low signal on T1, also militates against a malignant bony pathology.
These features, coupled with a history of anticoagulant therapy, helps us to arrive at the differential diagnosis of recurrent hemarthrosis with erosive arthropathy, or alternatively pigmented villonodular synovitis. This is not possible to differentiate on imaging alone.
Dr Sebastian Fung is a musculoskeletal radiologist who undertook an MRI imaging fellowship in Hospital for Special Surgery in New York. He now works in Sydney at St Vincent’s Private Hospital and Mater Hospital.