Ben Keneally, National Home Doctor Service CEO says company's like his can improve care and save costs (sponsored)
After hours services have become controversial in the last few weeks with many GPs responding negatively to recent advertising awareness campaigns by some deputising groups,as not being conducive to proper care. Ben Keneally, CEO of our largest and fastest growing deputising group, National Home Doctor Service, argues here that the case for the expansion of such services is solid
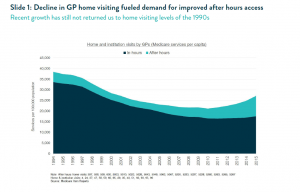
For much of the 1990s and 2000s, improving access to primary health care after hours was a key health policy objective. State and federal governments of all persuasions rolled out help lines, co-located clinics, workforce strategies and improved rebates and incentives with the intention of improving access to care and reducing pressure on hospital emergency departments. The genuine community demand for better access to after hours care was fuelled by a significant decline in home visiting by GPs during this period. (See slide 1).
The good news is that all this effort has now started to pay off. Access to after hours primary care has improved and there is now evidence the pressure on EDs from low acuity presentations has moderated, delivering savings to taxpayers.
The turning point
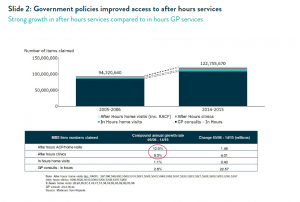
The turning point for improved access to care was the Howard Government’s “Round the Clock Medicare” package of 2005 which increased rebates for after hours consultations. Then came the 2007 extension of these increases to the “transition” period of 6-8pm on weekdays. These changes made fee-for-service funding of after hours practice more viable and encouraged ongoing innovation and investment by the private sector.
Since then, after hours clinic visits have grown at a compound annual growth rate of 8% and after hours home visits have grown at 12%2 (Slide 2). However, it should be noted that the total level of home visiting now occurring is still below the levels of 1995 (as can also be seen on Slide 1), and that after hours home visiting represents only 11% of all government spending on after hours health care.3
Reduced pressure on EDs
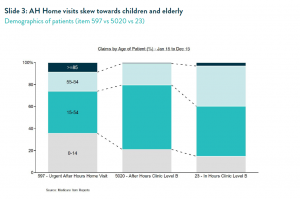
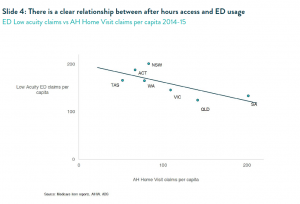
Improved after hours access to primary care, especially through after hours home visits, has helped reduce the pressure on hospital EDs. After hours home visits skew strongly towards children and the very old4 (Slide 3), who are also more likely to present at EDs. Over the last four years, low acuity presentations to hospital EDs nationally have grown at only 1.4% per annum.5 We also observe a very clear inverse relationship at a state level between the penetration of after hours home visiting and the rate of low acuity presentation at hospital EDs6 (Slide 4).
This diversion from hospital EDs not only delivers more appropriate care it generates clear savings for taxpayers. The weighted average cost of a low acuity ED presentation is $4407 compared to $130 for a home visit – and this excludes any of the costs associated with ambulance usage. The state by state comparison shows that for every additional home visit per capita, approximately 0.4 low acuity ED presentations are saved. This is consistent with our internal patient survey data in which around 40% of patients tell us their only alternative would have been to present to ED.
Case study: Gold Coast vs Central Coast
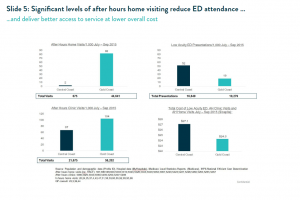
A more detailed case study makes the case even more explicitly. We compared the QLD Gold Coast to the NSW Central Coast which have similar demographic profiles, similar geography and access to two major public hospitals. However, the Gold Coast has one of the highest utilisation of after hours services and the Central Coast has a much lower rate, below the average for a metro area8.
Residents of the Gold Coast during the winter quarter of 2015 received 82 after hours home visits per 1000 residents compared to only 2 after hours visits per 1000 residents in the Central Coast. Similarly Gold Coast residents had 104 after hours clinic consults per 1000 compared to only 67 on the Central Coast. However, Central Coast residents were more than two and half times more likely to visit the hospital emergency department for a low acuity issue9 (Slide 5).
Based on reported Medicare expenditures and the national efficient hospital costs for Tier 4 and 5 presentations to ED, we can calculate that the cost per citizen of after hours and low acuity ED services on the Gold Coast is ten per cent lower than on the Central Coast, despite Gold Coast residents having almost twice the level of total access to services. Put simply, this shows what we know to be true: that good access to primary healthcare is much less costly than using hospitals.
The other good news to emerge from the case study is that better access to after hours care does not appear to compromise utilisation of daytime GPs, with the regions experiencing almost identical usage of daytime clinic consultations (Slide 6).
A government policy success
The growth of after hours home visiting over the last few years represents a success for government policy. The Review of After Hours Healthcare by Professor Claire Jackson found that after hours services “are recognised as having a critical role in meeting after hours needs, providing valuable support for GPs already working long hours, access to home visits and in many cases good continuity of care.” 10 However, the Review also raised concerns regarding the rate of growth of after hours items.
The current analysis puts those concerns in context and demonstrates that out of hours medical deputising services are delivering a positive policy outcome that is improving access to care, reducing pressure on hospitals and saving taxpayer funds.
This is an edited whitepaper authored and posted by Ben Keneally, Chief Executive Officer of National Home Doctor Service and Dr Umberto Russo ,General Manager, Clinical Governance, National Home Doctor Service. It was posted by NHDS with the approval of Medical Republic. It is appearing on the newsletter as a sponsored item.
(Endnotes)
1.
Slide 1 – Medicare item reports – http://medicarestatistics.humanservices.gov.au/statistics/mbs_item.jsp 1994-2015 for selected item numbers (597, 598,599, 600, 5003, 5010, 5023, 5028, 5043, 5049, 5063, 5067, 5220, 5223, 5227, 5228, 5260, 5263, 5265, 5267, 4, 24, 37, 47, 58, 59, 60, 65, 20, 35, 43, 51, 92, 93, 95, 96)
2.
Slide 2 – Medicare item reports 2005/06 and 2014/15 After hours home visits (inc. RACF): 597, 598, 599, 600, 5003, 5010, 5023, 5028, 5043, 5049, 5063, 5067, 5220, 5223, 5227, 5228, 5260, 5263, 5265, 5267 After hours clinics: 5000, 5020, 5040, 5060, 5200, 5203, 5207, 5208, In hours home visits: 20, 24, 35, 37, 4, 43, 47, 51, 58, 59, 60, 65, 92, 93, 95, 96 GP consult: 23, 3, 36, 44
3.
Medicare item reports 2014/15, Report on Government Services 2015, Commonwealth Budget Papers 2015, Health Direct Australia Financial Reports 2014, AIHW Australian Hospital Statistics – Emergency Department Care 2014/5
4.
Slide 4 – Medicare Item Reports data Jan 2015- Dec 2015 for items 597, 5020, 23
5.
ED low acuity presentations data from AIHW Australian Hospital Statistics: Emergency Department Care 2010/11, 2011/12, 2012/13, 20113/14 and 2014/5. Note growth rate calculated after grossing up reported low acuity presentations by state for the estimated proportion of total presentations covered by the statistical reports as reported by the AIHW in same reports – see for example table 2.2 on p10 of the 2013/14 report.
6.
Data as above for 2014/15 (AIHW and Medicare Item Reports); state population data from ABS
7.
IHPA – National Efficient Cost Determination 2014/15 – average calculated using the national efficient costs for Tier 4 and 5 ED presentations, weighted based on volumes of presentations and admissions by acuity tier
8.
National Health Performance Authority – “Healthy Communities 2011”
9.
Medicare Local Statistics Reports http://medicarestatistics.humanservices.gov.au/statistics/med_locals.jsp – and reported ED presentations from MyHospital website
10.
“Review of After Hours Healthcare” by Professor Claire Jackson