Plus how to manage TIAs and carotid stenosis in general practice.
Is it symptomatic or asymptomatic?
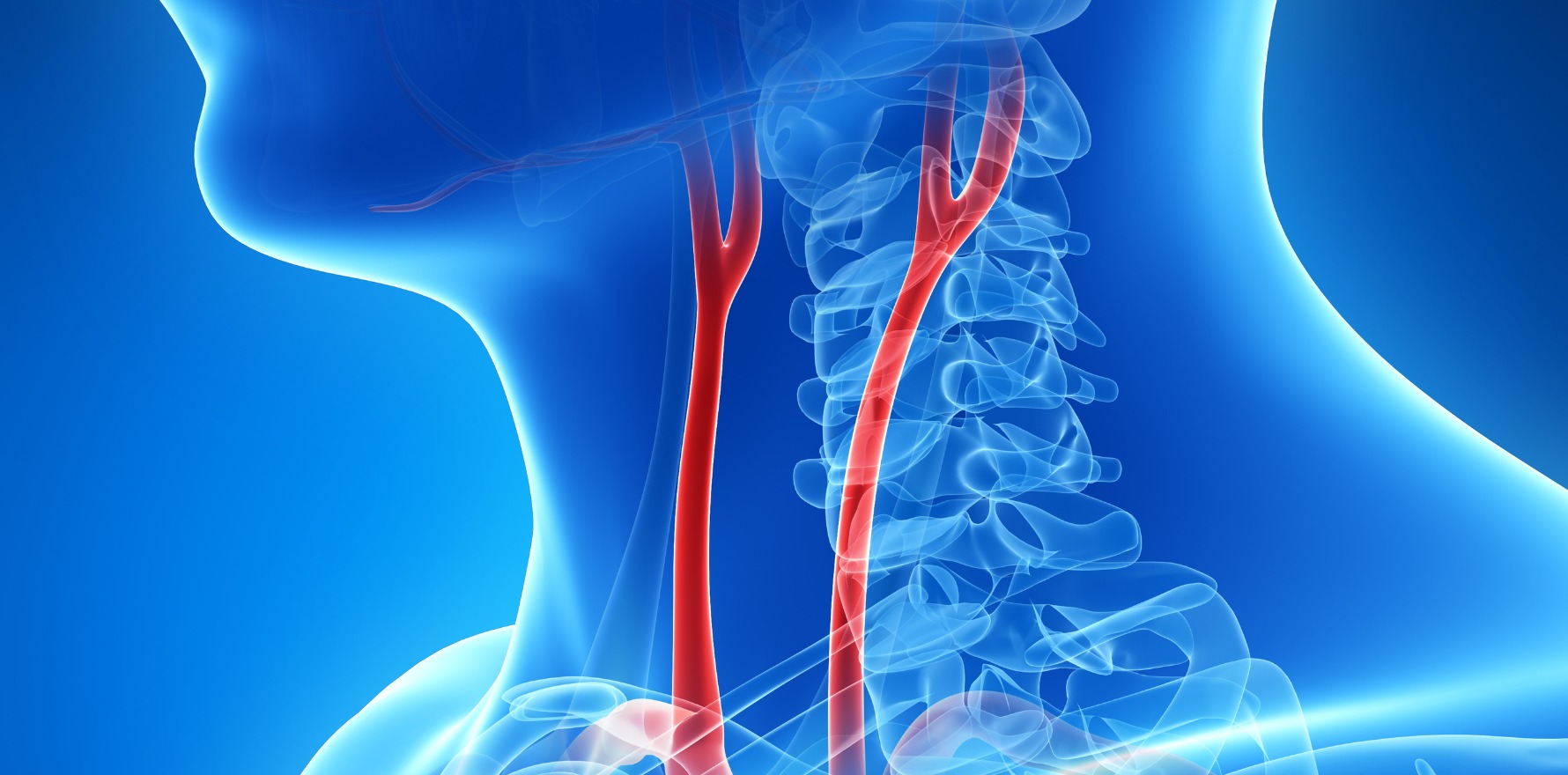
Carotid stenosis is defined as symptomatic when there’s a focal neurological deficit in the brain supplied by that carotid artery, according to Dr Shannon Thomas, Vascular Surgeon at the Prince of Wales Hospital.
Patients with symptomatic carotid stenosis will experience focal neurological and/or ocular symptoms that are sudden in onset and include one or more transient ischaemic attack (TIA) or ischaemic stroke within the previous six months.
Asymptomatic carotid stenosis typically presents as a bruit on examination and is defined as atherosclerotic narrowing of the proximal internal carotid artery by at least 50% in patients with no history of recent (within the last six months) ischaemic stroke/TIA involving ipsilateral carotid territory.
Dr Thomas cautions against causing undue anxiety around asymptomatic carotid stenosis. For patients with a less than 70% asymptomatic stenosis, the 5-year stroke risk is less than 5%.
“Asymptomatic narrowing is not something that patients need to be anxious about,” he says. “I do see a lot of patients who are told, ‘Oh geez, you could have a stroke. You’ve got this narrowing in your neck.’ There is no timeline to this. It’s not imminent when they have an asymptomatic narrowing.”
Should we be screening patients for carotid stenosis?
With a prevalence of approximately 3% across the general population, Dr Thomas says that routine screening for carotid stenosis isn’t warranted. However, the prevalence jumps to almost 50% in patients with peripheral arterial disease and other risk factors, such as hypertension and diabetes, making this an important patient group for GPs to consider screening.
“In your patients who’ve got peripheral arterial disease and other risk factors, they should be having some form of imaging to determine if they have a carotid plaque as well. We know that when you’ve got a carotid plaque it does increase your risk of having cardiovascular disease or having a bad cardiovascular outcome.”
Dr Thomas adds that while around 8% of all ischaemic strokes are a result of the carotid artery, all stroke patients will be investigated for carotid narrowing because the treatment is so effective at preventing further strokes.
Investigations
Dr Thomas recognises the important role GPs play in the management of patients who suffer a TIA.
“It’s important to try and get the workup and referral correct. Just because someone has had a TIA rather than a stroke, doesn’t necessarily mean that they’re home free, that the problem is past ― they still need to be actively managed,” he says.
Dr Thomas recommends duplex ultrasound as the first-line investigation for carotid stenosis. He says it’s very safe, it can’t dislodge the plaque, there’s no irradiation and it’s highly informative — allowing you to see the characteristics of the plaque and the speed and direction of blood flow.
“Duplex is very important in that it’s non-invasive and it actually gives you a lot of information about the carotid artery. It gives you a lot more information than just the degree of stenosis,” Dr Thomas explains.
“We can work out just how much blood flow is getting up to the brain, whether there’s enough perfusion pressure or not, and these things then directly correlate to stroke risk.”
He says it’s particularly important to have a specially trained vascular sonographer who can pick out the subtle signs that correlate to stroke risk.
Other investigations include:
- CT Brain (non-contrast) to determine if stroke has occurred and if so, whether it is haemorrhagic.
- Follow-up with CT angiogram if satisfied that no haemorrhage is present (this enables imaging of the carotid arteries at the same time)
- Routine bloods and BSL
- ECG to look for atrial fibrillation
- MRI if there’s an evolution of symptoms or history is unclear
Any suggestion of repeated symptoms, no matter how vague, should be an indication for repeated brain imaging and neurology review.
Treatment options
Treatment options include carotid endarterectomy, carotid artery stenting and the more recent procedure, trans carotid arterial revascularisation.
Dr Thomas says trans carotid arterial revascularisation takes advantage of the benefits of both carotid endarterectomy and carotid artery stenting without some of the risks.
“In the literature, the rates of stroke are less than 1%. We’ve started a program at Prince of Wales to do this and we’re getting very good results as well. And I think you’ll find over the next five years that more and more patients are done this way,” he says.
When to intervene?
Studies in symptomatic patients include ECST and NASCET and show that, generally, the benefit of surgery outweighs the risk in patients with severe stenosis (≥70%), with research ongoing for those with moderate stenosis (30-69%).
“We know that surgical intervention in these patients reduces their risk of subsequent stroke, that’s number one. And number two, it also allows for some recovery of the ischaemic penumbra ― that is brain tissue that is sort of hibernating and with increased blood flow will come back to life.”
A specific group of asymptomatic patients who may benefit from surgery are males, aged <75 years, with >5-year life expectancy according to the ACST and ACAS studies. The benefit of surgery in asymptomatic females remains unclear.
Asymptomatic carotid stenosis should be followed with regular ultrasound scan, particularly when there are features suggestive of potential plaque change (e.g. heterogenous plaque contents, ulceration of the plaque). Stenotic progression of an asymptomatic carotid stenosis may be an indication for treatment, in well selected patients.
Key points
• Patients with TIA need active management
• Patients with peripheral arterial disease and other risk factors should be investigated for carotid stenosis
• Asymptomatic carotid stenosis is not a cause for panic
• Surgical treatment of symptomatic carotid stenosis is very effective
Dr Shannon Thomas will be covering this topic in more detail at Healthed’s free webcast on 30 April. Register here to attend.
Note: This article was first published on 12 October, 2023
How do the CPD options work?
- Attend the webcast and earn 2 hrs CPD in the Educational Activities category by attending the webcast lecture and completing the evaluation (RACGP & ACRRM approved)
- Complete the optional post-webcast quiz and earn 0.5 hrs CPD in the Reviewing Performance category (RACGP & ACRRM approved)
- Complete the optional Patient Case Review and earn a further 0.5 hrs CPD in the Reviewing Performance category (RACGP approved*)
- Undertake the optional Micro Audit and gain 1 hrs CPD in the Measuring Outcomes category (RACGP approved*)
- We are working with the ACRRM to have the Patient Case Review (RP) and Micro Audit (MO) approved for its members as well, however ACRRM’s approval processes are somewhat slower! Until then, ACRRM members can claim the same CPD as last year.
Other professions can self-claim up to 4 hrs CPD.
Attendees will receive Certificate of Attendance approx. 4 weeks post-webcast.
Emma Henshall is a medical writer and a past president of the Australasian Medical Writers’ Association.