This idea could bridge our old and new digital health ecosystems, and maybe even our hospitals and primary care.
From little things…
The recent debut of Halo Connect may have passed with too little fanfare, given what the product might actually mean for our health system moving forward.
The product announcement itself was reasonably low key: a single FHIR-Open API based integration layer for our largest national primary care patient management system (PMS), Best Practice (BP).
It means that all those integrations to BP (there’s about 100 of them), which is probably somewhere north of being on the desktops of 60% of our GPs, can build their own APIs to talk to this “middleware”, and after that they largely can get on with developing their IP and not worry any more about upgrading versions to make sure they connect properly with BP.
As a one-off build for all those integrators, it should end up paying back very quickly.
For any new integrators it will make things a lot easier.
All this is the first part of the Halo idea.
It’s good for all those apps trying to integrate with BP, and obviously, it’s good for BP too, as integrations won’t keep breaking down. Usually when they do it’s not BP’s fault, but they will get the help desk call.
It will also put less stress eventually on all the on-premise versions of BP (it’s mostly still all on-premise) as their won’t need to be anywhere near the amount of reversioning work to keep all the integrations working smoothly.
So far so good.
But BP optimisation, believe it or not, is not the main long-term game of Halo Connect.
This despite BP being the biggest shareholder in the company developing the product.
The idea according to Chris Smeed, who is the CEO of Cubiko (one of the big BP integrations) and the person leading the development of the product in the new company, is to develop a platform that can act as the “middle woman” on all important point to point data sharing between major medical software systems.
It’s a big vision, but it’s not out of order.
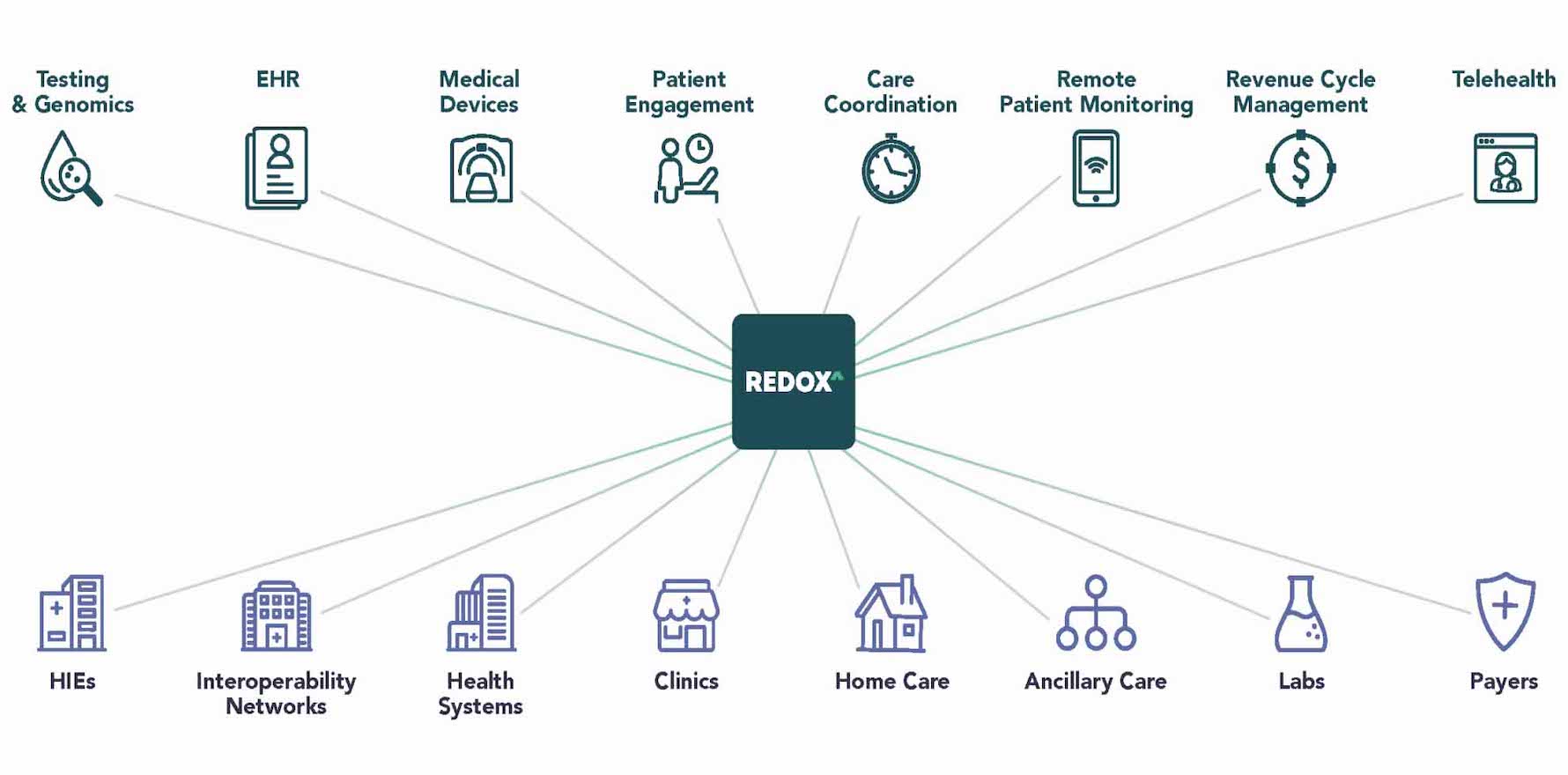
Middleware vendors of the sort Smeed is thinking Halo Connect might end up emulating are now experiencing massive growth in the US, where FHIR and Open API data sharing between providers has been mandated in law since April last year.
Despite being the law, and having more than 90% of software vendors and providers with robust FHIR and Open API interfaces so they can share data, the realities of FHIR and data sharing are necessarily complex. As a result a whole new industry segment of middleware vendors started to form in the US and grow rapidly. They act in the middle almost soley to connect one FHIR interface instance to another between providers and even vendors.
A good example of such a company is Redox. Unsurprisingly their tagline is “Interoperability for All” and their subline to that is “connect your product to any EHR”.
It obviously isn’t as simple as that, but if you take those two descriptors it gives you a good sense of what Smeed’s vision for Halo Connect is in Australia.
It’s a pretty big vision.
Notably, BP and Halo Connect probably are behind a few others in the concept and having a working version of a FHIR open API integration platform. Genie with its Gentu product has had this idea and offered FHIR based integration for its market platform for a while now. MD also has some form of FHIR integration it can offer partners.
But Halo Connect is technically independent of its PMS partner BP and has an intent to be an independent connection platform for the market. That’s a different approach so far to Genie and MD.
Halo Connect is obviously a long way back in the line product wise to something like Redox, given the huge leap ahead of Australia the US took many years ago by mandating data sharing standards for vendors and providers.
But in a sense, it might be much more important for platforms like this one to start evolving in Australia now, because Australia’s digital health ecosystem remains mired in a lot of isolated on-prem, non cloud based systems, which need connecting in a much better way than they do now – see old-technology concepts like “secure messaging” which we still rely on a lot in Australia but which is all but disappearing overseas.
The other thing we need a workaround for, until we can get our act together and start aligning all points of the system onto cloud based platforms, is how hospital EHRs connect to GP EHRs (or PMSs as we are calling them above).
At the moment they don’t connect at all really (some hit-and-miss secure messaging projects create some connection but not good ones for appropriate data sharing), and if we wait for everyone to get to the cloud like they are in the US, we will be waiting far too long – it will probably take at least 5-10 years from here in Australia.
In the meantime, ideas like Halo Connect might make for a reasonable workaround on this problem. A sort of bridge between various old technology systems until enough vendors and providers move to more modern data sharing technology.
This isn’t something that the Halo Connect people are saying they are thinking about in the short term, but when asked, they do say it might make tertiary to primary care data sharing and a longitudinal patient data journey between those domains much better than it is currently. Halo Connect would not be storing any of this data. It would just be the platform providing the connection.
At the moment, most hospitals are in a post-covid frenzy of building out virtual care capability.
But they all have a big problem. When their patients leave and go out into the community the best way to manage them is via the local GP network. They can’t do that easily because GPs are stuck in on-prem PMS islands (ie, our major GP PMS systems don’t connect easily to other systems to share data).
The Halo Connect idea, iterated enough, might be able to start doing this, so a hospital wanting to follow their patients out into the community could connect and talk to their local GP networks with much more ease.
After that, they just have a funding problem. Who pays the GP for helping out a hospital?
Smeed says that Halo Connect will also eventually attempt to act in the middle between primary and tertiary care and aged care (aged care hasn’t got a lot of tech to connect to yet, notwithstanding).
Hopefully our new federal government is going to tackle the problem of GP funding between hospitals and the federal government in some way soon.
Standing back a bit, you can imagine that with this middleware tech, and some sensible funding shifts (ie, send more money to the states to start working more effectively with our GP networks), that we might be able to seriously start tackling our lack of interoperability in Australia, a long way before we can manage to update everyone to more modern cloud-based web-sharing data technology.
Of course, there are some interesting commercial implications that arise from Halo Connect in the software vendor community.
Halo Connect is more or less a JV between BP, Smeed and the data analytics group, Aginic Ventures, with the majority of shares being held by BP. They’ve put in quite a bit of money each to get it started as well, so it’s a serious tilt they are taking at the idea.
Both Smeed, and BP’s representative on the Halo Connect board, Best Practice Chief Product Officer, Danielle Bancroft, see the future of the product and the company as a neutral platform play. They both would like to see it start connecting the major GP PMS vendor systems, where there is a need for such a connection, in addition, to connecting to major hospital EHR vendors one day.
Bancroft says that the product will be an important stepping stone for BP integration partners and their GP clients to eventually having a full cloud product. She doesn’t see why it can’t be that for competitors to BP as well. Halo Connect is after all a separate company with very different objectives and plans to BP.
It’s not entirely clear if there would be upside in joining up in the end for major competitor Telstra Health’s Medical Director.
In the end, if the federal government goes the way the US has gone, and somehow mandates sharing to a set of standards between vendors and providers, the system will end up with all the major PMS vendors talking more or less seamlessly to one another regardless.
It’s just that Telstra Health might want to try their own middleware connector platform play themselves. It might end up being a lucrative sideline – or the main game even one day.
There’s probably room for a few middleware companies, even in Australia, given the likely emerging complexity of connections between FHIR based application integrations.
Luckily Australia is a minnow and backward to date, so it doesn’t feel likely that a Redox would want to operate here. But if they did, they’d likely have quite a jump on the locals, given they already have integrations to all the major US based hospital EHRs and primary care PMS systems.
They might end up taking a stake in one of the local middleware startups.
In any case, Halo Connect is a fascinating market development for Australia. It indicates that in the absence of government providing a framework, the local software vendors are prepared to take a big step anyway.
It’s possibly not surprising BP is stepping out first with the idea of a neutral connection product (MD does have its own FHIR integration layer for partners).
Sharing and open systems are the inevitable future that we can all see now in more advanced digital health countries like the US, Denmark and Israel.
Taking a lead in this trend – breaking the old paradigm of not openly sharing data easily – is exactly what market leaders should be doing in Australia.
Note: If this story is of interest to you, Halo Connect and BP will both be at the upcoming Wild Health Summit on “No better time to align healthcare policy reform with technology reform”, and will be doing a short TEDx case study demonstration of the concept. Register HERE.