Prescription opioids are behind most fatal overdoses, prompting calls to treat the emergency reversal medicine the same way as glucagon for patients on insulin.
Experts are calling for routine co-prescribing of naloxone for patients on strong long-term opioids to tackle the growing death toll from prescription opioids in Australia.
Opioid-overdose deaths have doubled over the past two decades, but some of those lives could have been saved if patients had access to a PBS-approved medication, according to GP Pallavi Prathivadi and Associate Professor Suzanne Nielsen, who is deputy director of the Monash Addiction Research Centre.
“Take-home naloxone for people on opioids is analogous to intramuscular glucagon for patients with diabetes on insulin, or auto-injectable adrenaline for anaphylaxis,” they wrote in an MJA perspective.
“Most people are unlikely to need these emergency medications, but in the case of profoundly dangerous adverse events, naloxone, like glucagon or adrenaline, has a life-saving role.”
The CDC had already recommended that US doctors prescribe opioid antagonists for at-risk patients with chronic pain. This included patients who take either an oral daily morphine equivalent of at least 50mg, those prescribed both benzodiazepines and opioids, and people with a history of substance-use disorder or overdose.
Despite a lingering perception that naloxone was for people who used illicit opioids such as heroin, a 2018 report by the not-for-profit Penington Institute showed pharmaceutical opioids now accounted for the majority (roughly 70%) of fatal opioid overdoses.
Meanwhile, opioid overdose deaths rose almost 100% between 2002 to 2018 (from 482 to 900 per 100,000 Australians).
Previous research by the authors suggested almost 80% of Australians prescribed long-term opioids for chronic non-cancer pain fell into the CDC’s “high risk” category – meaning roughly 200,000 patients would be recommended take-home naloxone.
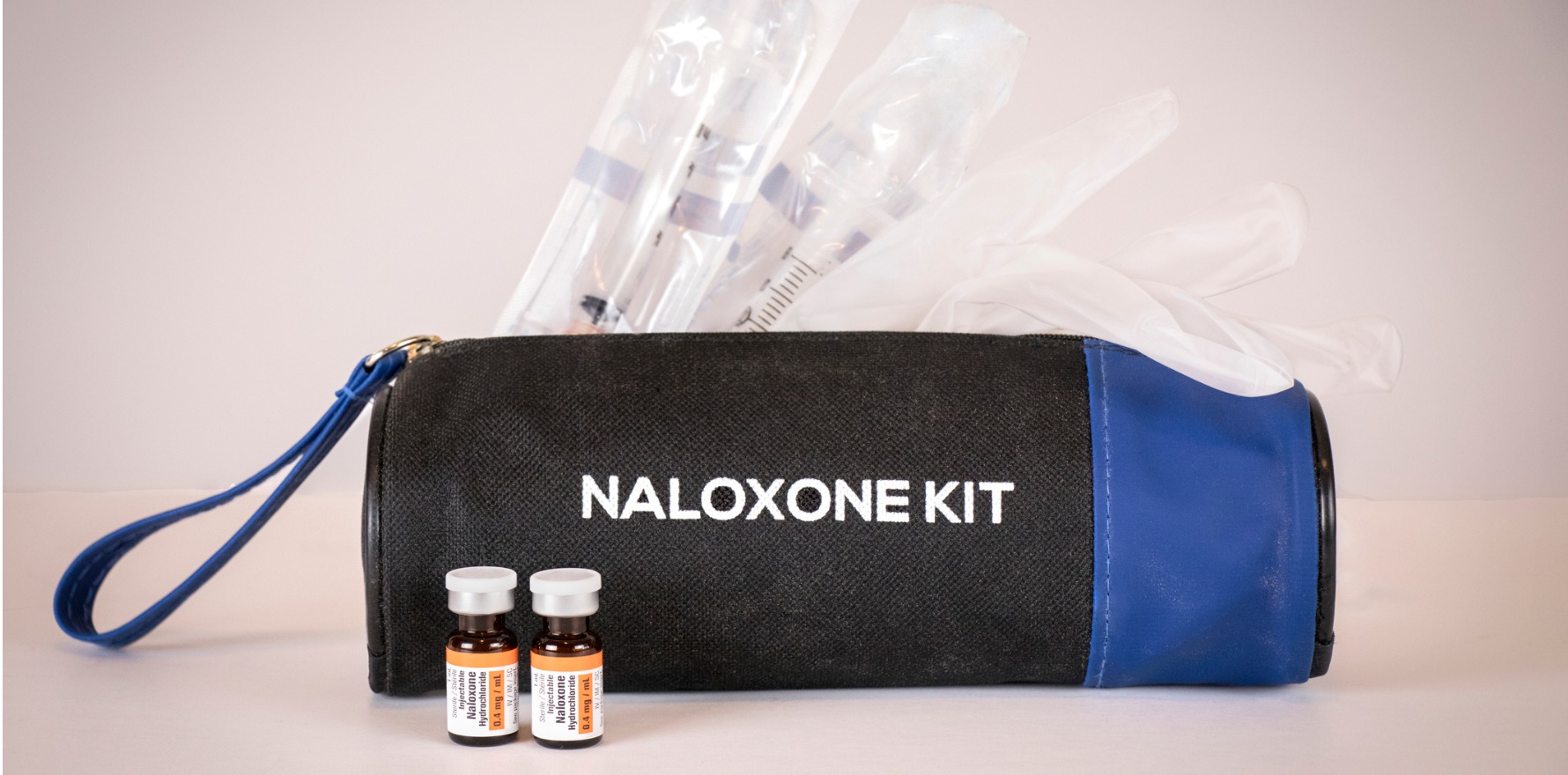
In Australia, naloxone is available as an intramuscular injection or nasal spray. Only the nasal spray is covered by the PBS, on an unrestricted General Schedule listing, but access is thought to be low.
Fewer than an estimated 11,000 units were supplied between 2014 and 2018, according to Dr Prathivadi and Professor Nielsen.
Currently, patients paid around $41 for the PBS-listed nasal spray, or $6.50 with a concession card. “This is comparable with the PBS cost of an adrenaline auto-injector or glucagon, which are both listed at $40.15,” they wrote.
When explaining a recommendation for take-home naloxone, clinicians could swap phrases such as “drug overdose” with “life-threatening opioid toxicity” or “severe opioid-related side effects” to avoid the stigma, they said.
NSW, WA and SA were trialling free take-home naloxone for people using prescription or illicit opioids who were at risk of opioid-related death or those who might witness an overdose.
Patient history of current opioid medications – especially at higher doses or slow-release preparations – and comorbidities such as mental illnesses or respiratory conditions could help clinicians identify patients who should carry naloxone.
Education on signs of opioid overdose would also be crucial for people expected to administer the medicine, said the authors.
“Most people prescribed opioids for pain are unable to identify common signs of potentially fatal opioid toxicity. Improved naloxone prescribing alone is therefore unlikely to be effective without education and increased awareness of opioid overdose signs by patients, family members, friends and carers.”
There was no evidence that prescribing naloxone would be seen as a “safety net” to justify high-dose opioid prescriptions, they added.
Read more: MJA 2021, 26 April