The scoring tool can bump people up or down a CVD risk category.
Coronary artery calcium (CAC) scoring in asymptomatic individuals may be beneficial, according to a new statement from the National Heart Foundation.
Its key practical use would be to reclassify patients without known CVD into either higher or lower risk categories, to augment the conventional absolute CVD risk assessment, the statement authors said in the Medical Journal of Australia.
“CAC scoring could be considered in people with moderate risk for whom management intensity is uncertain; for example, when the initial risk status is close to the threshold for high-risk status,” Professor Garry Jennings, chief medical advisor of the National Heart Foundation of Australia, and colleagues wrote.
A higher amount of calcium found in the coronary arteries during a CT scan was indicative of atherosclerosis and studies have linked it to a greater risk of cardiovascular events.
“I think it is fair to say that it is plausible that CAC may have important clinical benefits in some settings, but this has yet to be well demonstrated and it is also plausible that it may actually have little overall impact on hard patient outcomes.”
– Dr Michael Tam, GP and conjoint senior lecturer at UNSW.
But so far, the evidence has been weak and cardiologists were divided on the use of calcium scoring. Nevertheless, some doctors report finding it helpful in understanding the patient’s risk and treatment options.
GP Michael Tam, deputy chair of Sydney South West GP Link, warned clinicians to “not be overconfident in what are fundamentally limited recommendations based on low-strength evidence”.
“I think it is fair to say that it is plausible that CAC may have important clinical benefits in some settings, but this has yet to be well demonstrated and it is also plausible that it may actually have little overall impact on hard patient outcomes,” said the conjoint senior lecturer at UNSW.
While more information was still needed before strongly supporting the tool in asymptomatic individuals, the National Heart Foundation issued a new position statement outlining the latest evidence.
The four key recommendations were:
- CAC scoring could be considered for selected people with moderate absolute cardiovascular risk, as assessed by the National Vascular Disease Prevention Alliance (NVDPA) absolute cardiovascular risk algorithm, and for whom the findings were likely to influence the intensity of risk management.
- CAC scoring could be considered for selected people with low absolute cardiovascular risk, as assessed by the NVDPA absolute cardiovascular risk algorithm, and who have additional risk-enhancing factors that may result in the underestimation of risk.
- If CAC scoring was to be undertaken, a CAC score of 0 AU could reclassify a person to a low absolute cardiovascular risk status, with subsequent management to be informed by patient–clinician discussion and followed contemporary recommendations for low absolute cardiovascular risk.
- If CAC scoring was to be undertaken, a CAC score > 99 AU or ? 75th percentile for age and sex could reclassify a person to a high absolute cardiovascular risk status, with subsequent management to be informed by patient–clinician discussion and followed contemporary recommendations for high absolute cardiovascular risk.
The group came to these conclusions after reviewing the available evidence, which included a 2018 systematic review used by US health authorities.
There was conflicting evidence, with some studies indicating that CVD control and the risk of a major CVD event were improved, and others failing to find a clinical benefit.
“A recent analysis of about 1000 asymptomatic individuals with family history of early onset coronary artery disease demonstrated the potential of CAC scoring to reclassify risk in an Australian population,” Professor Jennings and colleagues wrote.
That study found that one in five patients who were labelled “moderate risk” using the Australian algorithm had CAC scores of 0. In contrast, three in four subjects who were first considered “low risk” using the algorithm had CAC scores above 100.
“The benefit of refined risk assessment is that more individuals can receive risk management interventions of an intensity appropriate for their level of absolute cardiovascular risk,” Professor Jennings continued.
“We posit that a CAC score of 0 could also reduce anxiety for individuals, and possibly also their clinicians, who are reluctant or unable to tolerate more intensive risk management therapies otherwise indicated by their initial absolute risk assessment from the NVDPA algorithm.”
Dr Tam said GPs needed to be especially careful when treating those classified as having “moderate” absolute cardiovascular risk on traditional risk calculators.
“Simply, most people will end up in this category at some point simply due to age, and the evidence simply does not support the use of CAC as a de facto screening tool,” Dr Tam said.
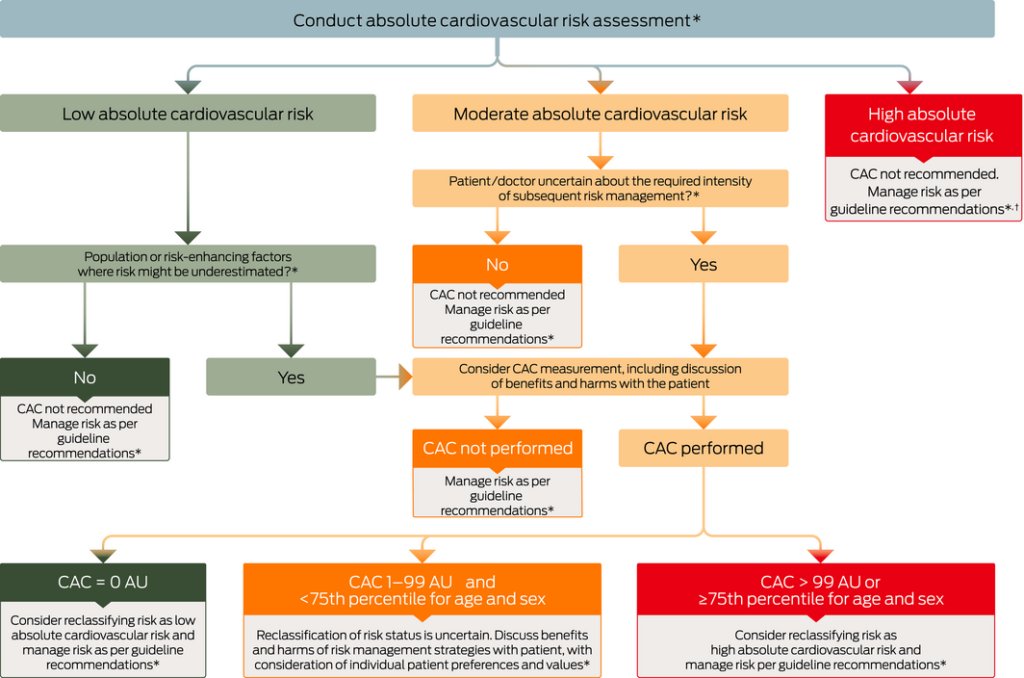
Some other practical advice from the National Heart Foundation authors included suggestions to assess CVD risk on clinical grounds before CAC scoring. High-risk individuals would not need additional CAC scoring to reclassify their risk. But there should also be caution about underestimating the risk among people with a CAC of 0 AU but with other high-risk factors.
“The 2012 NVDPA absolute risk algorithm may underestimate risk in certain populations, such as Aboriginal and Torres Strait Islander peoples, or in others with known risk-enhancing factors not fully captured in the NVDPA algorithm,” the authors said.
“CAC scoring could be considered in some instances to reclassify risk.”
Read more: Vulnerable plaque is dead, long live vulnerable patients