Individual doctors are usually not at fault when mistakes are made in the delivery of healthcare
Individual doctors are usually not at fault when mistakes are made in the delivery of healthcare services
In Australia, estimates suggest undesired harmful effects from medication or other intervention such as surgery, known as “adverse events”, occur in around 17% of hospital admissions. This results in up to 18,000 unnecessary deaths and 50,000 temporarily or permanently disabled patients each year.
Over 50% of adverse events are the result of medical error. Harms are physical, financial and psychological. Adverse events mean patients need to stay in hospital longer, have more treatment and incur financial loss.
Adverse events are the result of errors and violations (deviations from prescribed practice) of health-care professionals. Although the direct and most obvious causes of adverse events are errors and violations, the causes of adverse events we can control are the working conditions and organisational systems that cause people to make mistakes.
When the pace of work is too fast, health professionals can get distracted and feel under pressure. When supervisors turn a blind eye to non-compliance, teams aren’t functioning well, equipment is unavailable or opportunities for training rare, the willingness and ability of staff to perform reliably is reduced.
Safety cannot be assured by identifying the individuals who make an error. Safety can only be assured by creating conditions in which people can perform well.
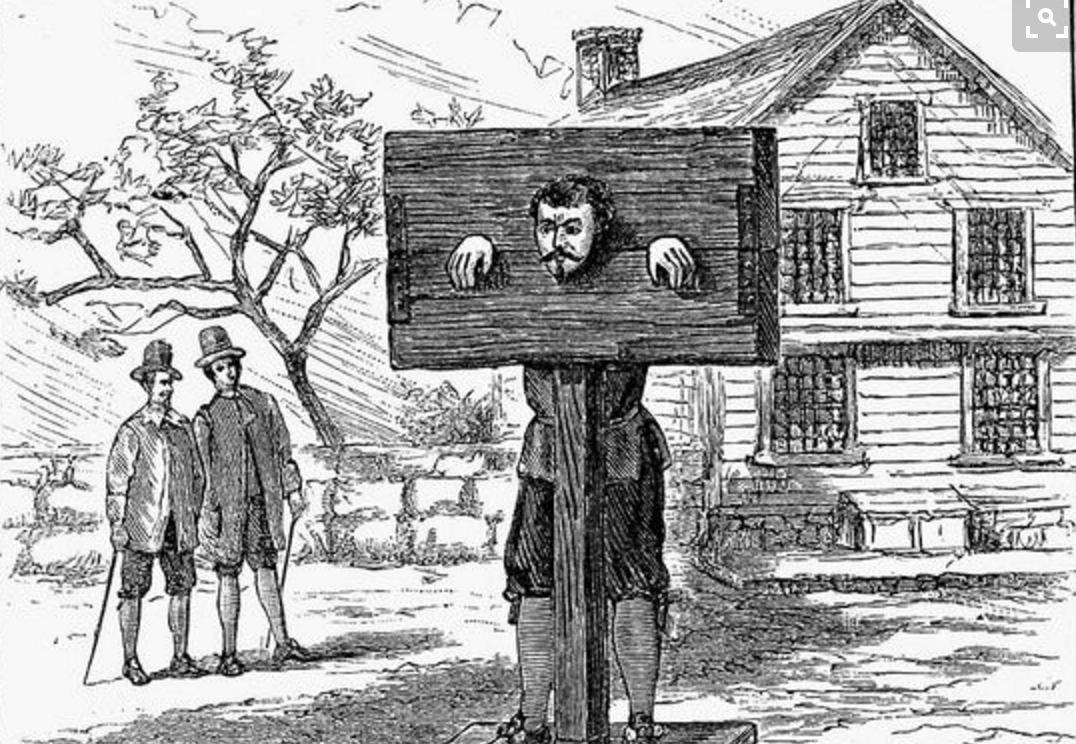
Blame is unhelpful
Finding someone to blame and dealing with this person by assuming they are uniquely incompetent (a person-centred approach) is a comforting strategy for those managing risk and for society at large. Much less satisfying is the notion that the majority of health professionals, in the same situation, would make the same mistake and that perhaps the situation, not the professional, is to blame.
The human tendency to blame others’ mistakes on their personal characteristics (ability, personality, attitudes) is even stronger when the outcome of the mistake is more severe (such as a patient’s life being shortened). This makes it difficult to move away from blame even when there is no compelling evidence “person-centred” strategies reduce error rates.
A person-centred approach also exacerbates the feelings of guilt, shame and anxiety that plague health-care professionals in the aftermath of error. These negative emotions, in turn, can lead to denial, avoidance and a failure to learn about the causes of the error. The possibility of putting preventive strategies in place is then limited.
The health-care professional may feel defensive, and this doesn’t help patients or their families learn the truth about what has happened and, in many cases, compounds the distress they feel. Blame means a lost opportunity for learning and can be detrimental to open and honest patient-professional discussions.
What are the alternatives?
Although we can and should focus efforts to reduce the number of medical errors made, errors are inevitable and so we also need to prepare for them more effectively. Both health professionals and patients need better support.
For health professionals, building psychological resilience at an individual and team level may help. Psychological resilience is defined as an individual’s ability to adapt to stress and adversity; to be positive, optimistic and to learn from mistakes. Not everyone is equally resilient and this is where being part of a team or being able to access social support from others is important.
So, what can we do in health care to promote resilience? At present, there is no definitive answer to this question; there is little research evidence available and even fewer recommendations.
In the United States, rapid response teams have been established in acute hospital settings to provide individuals with the support they need after an error. Support is offered either informally within the unit, through trained peer supporters within the hospital or via referral to professional guidance.
Training staff in emotional resilience is one approach that has been reported as successful among nurses transitioning from being students to staff. Mentoring for physicians has also been promoted as a strategy to enhance individual resilience and reduce burnout and stress. Neither approach has yet been evaluated at sufficient scale.
Minimising power differences between team members is important in encouraging people, no matter what their professional status, to speak up, ask questions and check understanding.
Training health-care leaders how to invite and appreciate contributions from all team members may provide a basis for greater equality and openness in health-care teams. When things go wrong in health care, blame is a rife but unhelpful response. What we need now are evidence-based strategies that support staff and organisations to use adverse events as an impetus for change.
Reema Harrison, Lecturer & Research Fellow: Patient Safety, University of Sydney and Rebecca Lawton, Professor, Psychology of Healthcare, University of Leeds
This article was originally published on The Conversation. Read the original article.