A lot has changed in two years, happily. The priorities now are to increase testing rates and reach unvaccinated at-risk people.
Stigmatising care, pain with inadequate relief, mixed messages on transmission, loss of money and privacy, and feeling like a lab specimen. These are a few of the experiences reported by men who contracted mpox just two years ago.
In-depth interviews conducted in 2022 show the tension that can exist between patient-centred care and public health when health systems are confronted with a novel contagious illness – especially on the back of a worldwide pandemic.
The worst accounts of dehumanising care are reminiscent of the early days of the AIDS crisis almost 45 years ago.
Now mpox is back, and the numbers are already more than six times the 2022 total with 905 cases across Australia, according to the National Notifiable Disease Surveillance System.
But while the numbers are higher the news is better: thanks to an effective vaccine and improved understanding around transmission, both disease severity and the psychological and social impacts of mpox should be lessened this time around.
There is no longer a requirement to isolate at home for three weeks, for example, as it has become clear that nearly all transmission is through sexual contact rather than airborne or via droplets.
An infection is considered no longer transmissible if lesions have scabbed and the scabs fallen off, or in cases with no lesions, when all other symptoms have resolved. Until then, the advice is to minimise transmission risk by not having sex or intimate contact, sleeping alone, covering lesions with clothing or bandages when going out, practising good hand hygiene, masking if there are any respiratory symptoms and avoiding pregnant, immunocompromised and very young and very old people. Contact tracing is also important where possible.
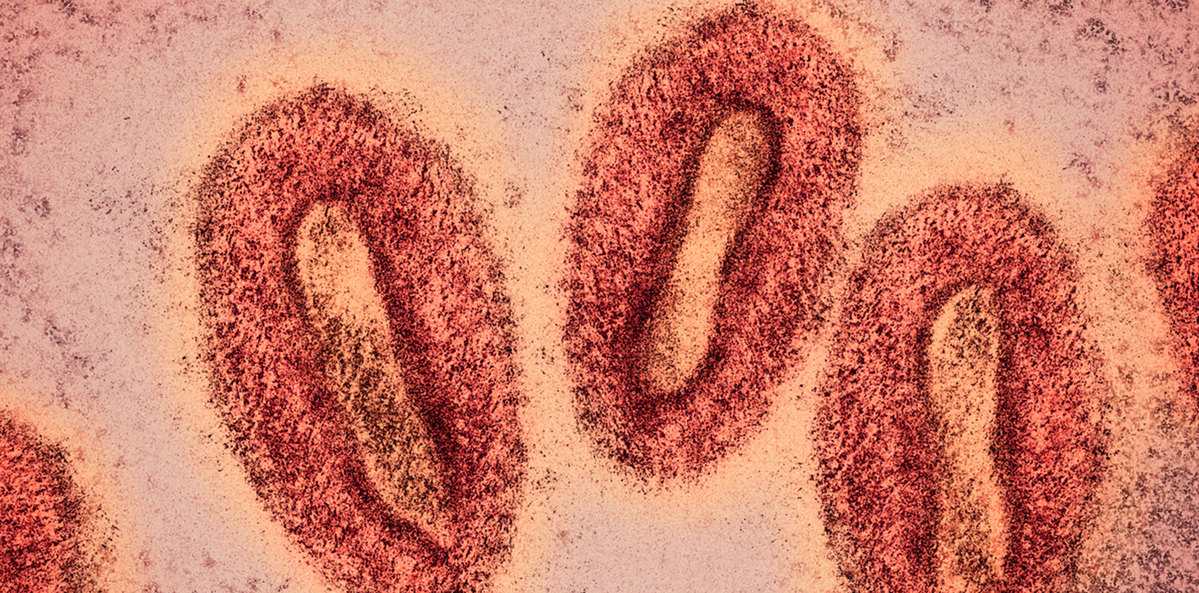
Dr Phillip Read, director of sexual health in South Eastern Sydney LHD and director of Kirketon Road Centre, says the vaccine has driven the main changes in presentation this year compared to 2022. Around a third of cases now are in people who have received Jynneos (two doses, available free at sexual health clinics) but their symptoms are markedly less severe.
“They are extremely unlikely to be hospitalised compared to unvaccinated persons, and their symptoms tend to be much milder, with fewer systemic symptoms, and much more likely to be just localised to the genitals,” Dr Read tells The Medical Republic.
“It can be a couple of pimples, it can be just anal irritation, it can be a relatively small ulcer – compared to the very dramatic photographs that we all saw a couple of years ago.”
A research letter in JAMA Network Open this month describes a significant waning in antibody levels a year after vaccination. If antibodies are a good correlate for immunity, that would make a case for boosters, contrary to interim advice given by ATAGI in August.
But Dr Read, noting that the study is limited to antibody counts, says it is much more important to reach the under- and unvaccinated than to give boosters.
“GPs and other people really need to be alert for who could be eligible for vaccine,” he says, adding that the further people live from the inner city, the less likely they are to be vaccinated, especially those from CALD backgrounds.
“Although [the vaccine] may or may not completely confer total immunity to the infection, it absolutely is still mitigating disease severity and outcomes for those individuals.
“About 65% of the cases are in people who have either had no vaccine or only one. So while a booster may at some point be recommended as the evidence emerges, I think our public health priority is probably reaching unvaccinated or partially vaccinated individuals, because we know they are at worst risk of a poor outcome.”
Lifting testing rates is another priority, Dr Read says, as currently the positive test rate is around 30%. Mpox is a notifiable disease and a positive PCR test is required for notification. Laboratories are running the test almost every day and results are usually a one-day turnaround, geography permitting.
“We need to be very liberal with whom we offer the testing to with mild symptoms,” he says. “We’re very much encouraging people to send tests for any suspicious or even mildly suspicious lesion … If you’re thinking about an HSV test, you should be thinking about doing an mpox test as well.
“The tests are highly reliable and relatively sensitive, although it is worth repeating for a highly suspicious lesion if the initial test comes back negative.”
‘Like being gay is wrong again’
In 2022 as case numbers rose in Europe and the US, with a lot of Australians travelling overseas for Pride Month, Dr Anthony Smith from UNSW’s Centre for Social Research in Health, with colleagues Professor Martin Holt, Dr James MacGibbon and others, undertook a national survey to gauge the level of understanding around mpox.
Dr Smith followed the survey with a qualitative study to get a deeper understanding of patients’ experiences, interviewing 16 people (three of them carers) at time of mpox diagnosis and six months later to learn of any long-lasting effects.
A picture emerged in which healthcare workers were more focused on containment than patient-centred care, and where patients could feel like they were part of a scientific experiment, when they didn’t feel they were being shamed for their illness.
The public health concern and the need to investigate transmission routes are highly understandable given the novelty of the virus, especially in the wake of covid. But that same novelty also made the experience more frightening and traumatising for patients.
“There was a bit of an AIDS crisis framing, although it was not as bad in terms of morbidity,” Dr Smith tells TMR. “There was also the recency of covid-19, a sense of ‘Are we going through that again?’
“We know that gay and bisexual men experience stigma and discrimination in healthcare settings and in the general community, and that’s sometimes related to sexually transmissible infections and HIV in particular.”
There were some stories of “a really good doctor” or nurse who gave reassuring, appropriate and sensitive care, but for every one of those there was another who lacked patience and lacked understanding of the patient population.
One thing that made it harder to trust and follow guidance was the incongruence between the public health advice – which emphasised isolation and masking due to the risk of droplet or airborne transmission – and what men were reading for themselves, which was that transmission was primarily through sexual contact.
“When the advice you’re being given is to isolate three weeks in your home and not see anybody and not go outside, but all the other advice that you’re seeing – including in journals – is suggesting that it’s really sexual transmission that’s driving it, you start to lose a bit of faith in the guidance you’re being given and you adapt the decisions that you make,” Dr Smith says.
He says there was a great willingness among patients to protect others by restricting their own lifestyles temporarily.
But the insistence on three weeks’ isolation had serious impacts for people who could not work from home, both financially and in terms of privacy, as it required them to declare their illness to their employers.
“It made me feel … like being gay is wrong again,” one respondent told the team. “It put me under a lot of stress because I was new in my role and I’m not out to my employers, I can’t say I’m going into isolation … They would figure, ‘Ah, it’s monkeypox. Well, you’re gay and you’re this and that.’ I wasn’t ready for that.”
Dr Read says the isolation rules, no longer in place, were based on the existing literature on mpox from Africa, where presentation usually involved extensive lesions all over the body and mortality rates were as high as 8%.
“The advice then around isolation was very much framed around the existing state of knowledge at that time,” he says. “And people were isolated from their partners and couldn’t work.
“As [numbers grew to] 90,000 cases across the globe, the data quickly began to show that, in fact, transmission was limited to certain situations. The majority of people had more localised genital lesions than significant lesions elsewhere, and healthcare workers were less likely to catch it than we first feared.
“So I agree there was a strong approach at the start … I think the precautions now are much more reasonable and much more manageable and less stigmatising for individuals, so I’m pleased that they’ve been changed.”
Related
There was another incongruence in 2022, between the symptoms the clinicians were most concerned about and those that were most distressing for some patients. Despite the focus on droplet rather than sexual transmission, clinicians tended to focus only on lesions, given their correlation with transmissibility.
Some men had very few lesions but had bad fevers, myalgia and respiratory symptoms.
“There was one participant who was coughing up blood, and he didn’t feel the doctor took that seriously for the first couple of days,” Dr Smith says. “Whenever he spoke to them on the phone, they kept focusing on lesions, but he had one lesion that didn’t really worry him.”
Some of those who did have extremely painful lesions said they were offered only paracetamol, which “didn’t really take the edge off the pain”.
“There was one participant who had to beg for sleeping pills, because the pain from his anus was so bad that he couldn’t sleep,” Dr Smith says.
One especially harrowing episode of care happened overseas when a participant presented to emergency with agonising anal lesions and waited hours for pain relief.
“They put me in a side room,” this participant told interviewers. “They catheterised me with no pain relief, which was horrific … I got left in the side room for at least 6 hours, I was screaming in pain. I honestly would’ve rather died. It was almost like being an AIDS patient back in the ’80s. I felt so discriminated against.”
During his 10-day stay, this interviewee said, most of the nurses refused to change his bedding or remove waste from his room.
“The comparison with AIDS here appeared to be a way to express the profound sense of injustice and neglect within a healthcare setting,” the paper says. “In [this participant’s] case, this involved poor pain management, perceived judgement around his acquisition of mpox, and being isolated and neglected.”
Dr Read says experience has shown that the “risks to attending healthcare staff are relatively negligible”.
Pain relief – which he says not all patients require, especially when vaccinated – should start low with paracetamol and ibuprofen, non-steroidals and lignocaine gel for lesions. A few patients have required inpatient pain relief with opioids and a very few have been treated with the antiviral tecovirimat (Tpoxx).
And as for stigma and discrimination around LGBTQIA+ health, broadly and in the health system, Dr Read says “there is still, sadly, work to do”.
Dr Smith says the novelty of the virus in 2022 made it both “unfamiliar and therefore scary, but also unfamiliar and therefore a scientific mystery. And I think that led to clinicians either being a little bit homophobic or not managing their emotional reaction to this unfamiliar virus, or sometimes enjoying the medical mystery a bit too much.”
But Dr Read says a forensic or inquisitorial approach to finding information about drivers and transmission networks is what has allowed the guidelines to evolve into something more appropriate and humane for the disease.
What now?
The key messages are, on one hand, that we need to do more testing and more vaccination; on the other, not to forget the patient in the hurly burly of outbreak management.
Dr Smith acknowledges the huge taskload on clinicians, but says a little time spent listening to patients’ fears and questions goes a long way.
“There are, obviously, lots of things that clinicians are being asked to do all the time,” he says.
“The patient might be asking, how am I going to talk to work? Talk to my sexual partners? What sort of symptoms am I going to get? Am I going to end up with scarring?
“It might be that being diagnosed in 2024 is slightly less distressing than the 2022 outbreak, just because it’s a bit more familiar – but it’s still a scary disease.”