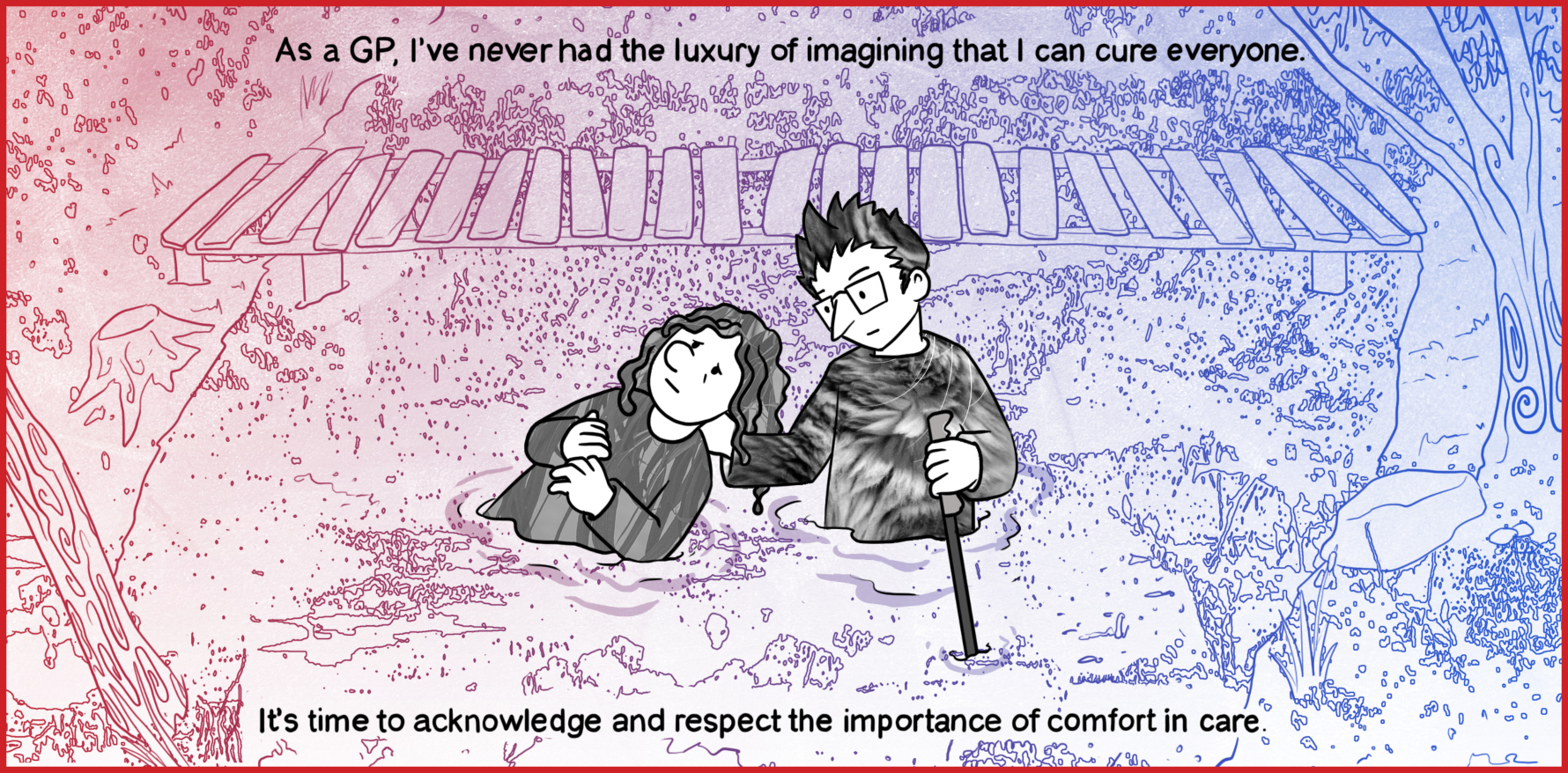
Patients can drown in the swamp. Keeping them afloat can drag us under if we’re not supported, funded and resourced.
In general practice, we have always been taught that our job is “to cure sometimes, to relieve often and to comfort always”. Our motto tells us to practice “with the head and the heart”. Of course, we fail individually and as a profession. Sometimes, we get caught up with the glitter of cure.
Cure is always the most attractive goal, of course. There will never be a Nobel Prize for the aged care worker who provides exemplary comfort. We fund research into the latest drug or app, but less into community nursing or the skill of providing comfort people need to face another day. It makes us feel better to focus on cure, because it helps us avoid the inevitability of suffering.
But when we are ill, we need people who are wise enough to look the horror of unfixable suffering in the face, and not retreat into protocols to make ourselves feel better.
Cure is a worthy goal, but it is unrealistic in chronic diseases. In mental health, the drive to cure shows itself with metastasising institutions, apps and protocols, all “evidence-based” and all designed to distract us from truly engaging with suffering. It shows up when CBT protocols are applied mindlessly, or when increasingly complex and experimental drug regimes are tried again and again and again – what we used to call “the elixir of desperation”. Worse, we create complex health systems that keep the consumer and carer busy bouncing around the pinball machine of care until they give up, all in the name of “doing something”.
Once patients give up, they become invisible to us. At worst, we assume they are cured, when in fact they just retreated because they are no longer able to bear accessing a system that invalidates their pain.
Just because they are moving, doesn’t mean they are recovering.
As a society, we get caught up in removing suffering, so comfort isn’t necessary. We want to believe that a drug or technique will remove suffering so we won’t have to bear it, not only as a patient, but also as a doctor. It’s one reason why some patients are discharged when the team feel they have “nothing to offer”. Care can be predicated on the treatments available, not the patient’s needs. We discharge them so we don’t need to look suffering in the face.
As a GP, I’ve never had the luxury of imagining that I can cure everyone. Other services discharge patients who are not getting better, or don’t have an illness that can potentially be cured. These patients end up with us. It’s hard, confronting, painful work but it is an enormous privilege.
I remember caring for a woman for decades who had motor neuron disease, and could only move her eyes. She taught me how to be with someone who cannot be cured, and to think deeply about what comfort really means.
This work is not seen or valued in policy, and is often disparaged by powerful people who gain status and power by generating cures.
One wrote recently that “the age of generalism, of non-specific payments for GPs to do something unspecified, is dead”.
I disagree, partly because, although my work may look “unspecified”, I can tell you exactly why I do what I do. It just may not use language or theoretical frameworks that are understood and accepted in other disciplines.
This work matters. Someone has to do the hard, relentless work of caring for the person who can’t read the app, doesn’t fit the protocol, can’t afford the treatment or can’t access non-GP care. Abandoning them is cruel.
First Nations people lead the discourse on suffering. In Western medicine, no matter what we create that plugs in, fits in a bottle, or standardises treatment, what we most need is the wisdom that comes from generations of engaging honestly with suffering. In my view, our deepest strengths come from the enormous wisdom of the aunties and uncles in our community. We need to be honest enough, and strong enough to admit that with all our knowledge and skill, at its core, what we all need is a wise auntie or uncle to be with us when we suffer and provide deep wisdom, comfort and care. Otherwise, health becomes a conveyor belt of interventions, requiring carers and consumers to commit to a career of regimens and appointments. This is disease management, not healthcare.
We can do better.
When patients are mired in the swamp, when we know they will eventually drown, when they have been abandoned by other services as being too complex, too demanding or too unfixable, the best we can do is be there. Sometimes, something will change, and the patient will find the strength to move on. Often they won’t.
There is ample evidence that being with suffering makes an enormous difference. It’s just not the sort of evidence that is heard or understood at a policy level. The shift to transactional care means it is often unfunded.
We need support to do this work. In my view, the reason we GP swamp guides need supervision and/or peer support is that these patients can drag us under. It is not their fault, but they do. Learning the skill of keeping upright while supporting someone who is drowning is hard. There are far too many of us drowning. Often this work is seen as “being nice” or “being kind”. This under-represents the wisdom, knowledge and the skill needed to do the work.
Early in my career, I ran a workshop on mental health attended by a colleague who knew me and my work very well. He approached me and thanked me for my contribution and then commented “I had no idea there was any theory behind what you do”.
There is theory, and it is the hiking pole that keeps us upright in the mire. If I had one piece of advice for swamp guides, I would say this – the reason I am still upright is decades of learning and a toolkit full of useful theories learned from dozens of wise teachers, mentors and supervisors. If I had stuck with “being nice” I would have gone under years ago.
For many colleagues on the high ground, this work can look like “doing nothing”, or “doing something unspecified”. I would argue that the ability to “specify” is not the arbiter of quality, but I digress.
There is deep work, under the surface, in “doing nothing”. From the high ground, I am simply standing there, and perhaps there is a sense that there is no point funding someone who is standing still. But just because you have no idea of the theory, skill and wisdom I am using, doesn’t mean it’s not there.
The people who are mired in the swamp matter. Their guides matter. The wisdom acquired by being with suffering matters. It’s the reason we became health professionals, to cure sometimes, to relieve often and to comfort always. It’s time to acknowledge and respect the importance of comfort in care.
Associate Professor Louise Stone is a working GP, and lectures in the social foundations of medicine in the ANU Medical School. Find her on Twitter @GPswampwarrior.
Dr Erin Walsh is a research fellow at the Population Health Exchange at ANU. Her current focus is the use of visualisation as a tool for communicating population health information, with ongoing interests in cross-disciplinary methodological synthesis.