the first in a series of articles on managing musculoskeletal pain, by Dr Dan Bates
This is the first in a series of articles on managing musculoskeletal pain, BY DR DAN BATES.
The article outlines a basic approach to musculoskeletal pain that grew out of a need to manage osteoarthritis for those facing joint replacement who were currently too young or too unwell for surgery, or who just didn’t want a replacement. It encompasses a sequential process that addresses the pain first (The Pain Pie), gets the patient exercising (Rule of 2’s) and subsequently aims to decrease weight (The 4H’s).
The Pain Pie
The Pain Pie is based on the idea that pain is generally not just a single sensation (although it can be). Pain is comprised of multiple sensations, from aching and tightness through to burning and electrical shocks. All indicate different things going on for the patient, all of which can be addressed separately to create a simple but comprehensive treatment strategy.
Pain is thought of as nociceptive (somatic or visceral), neuropathic or sensitisation. Put simply, nociceptive pain arises from a structure, neuropathic pain from a damaged nerve and sensitisation is the “volume control” which can turn pain off, or make it absolutely terrible.
Pain is exceptionally difficult for patients to describe. The Pain Pie is a “thinking tool” for identifying the features of pain. It splits musculoskeletal pain into nine key areas. Nociceptive pain (encompassing somatic, inflammatory, bony, myofascial, mechanical and ischaemic features), neuropathic pain or features, sensitisation and contributing factors. If the pie is used to visualise the patient’s pain, the ‘pieces’ can be seen as adjustable. Sometimes the patient’s pain is 80% neuropathic, with all other components squashed into the last 20%.
In this case just addressing their neuropathic pain or features may be enough. However, commonly, the patient will have features of pain across each ‘piece’ and you may need to address all features at a single time to get any significant improvement in pain. For example, the patient may have somatic pain with inflammatory, myofascial, and bony features in the setting of a moderate degree of sensitisation, with associated muscle wasting and weakness. Simply giving them anti-inflammatories is unlikely to have a significant impact on their pain. A more effective strategy may need to address their pain with some anti-inflammatories, adding massage and dry needling for the myofascial pain, a strength program for the muscle weakness and wasting, and some pregabalin in combination with education to address the sensitisation. This emphasis on a combined approach acknowledges the multifaceted nature of a patient’s pain, and, therefore, the multi-strategy approach often required to effectively address that pain.
Teasing out the patient’s pain starts with the usual questions of HOW OLD, WHEN and WHY. Each indicates different diagnostic possibilities. Clearly, for kids, growth plates and osteochondritis dissecans are primary issues, while degenerative disease comes to mind for older patients. If the pain has only been around for a day, bursitis, tears and fractures are flagged, while something that has been around for five years brings you back to degenerative disease, neuropathic pain and sensitisation. The WHY is generally the most interesting aspect. For degenerative disease, the trigger is generally “Nothing, it just started hurting one day”. Traumatic events are always very useful for pinpointing tears or fractures. With kids, if you are lucky enough to have had mum or dad filming a game, the mechanism commonly gives you the diagnosis. The final thing you are looking for is a change in what they have been doing; a new pair of shoes or racquet, new job, period of rest and then returning back into their normal level of activity. The opposite is also true, with multiple consecutive days of activity and no recovery time being a common trigger for overuse injuries.
‘Somatic Pain’
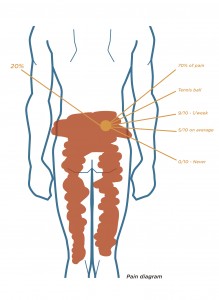
Somatic features of pain are aching, broad, heavy, soreness, sharp, or throbbing pain with referral into specific or non-specific areas. These features allow you to ‘Map the Pain’ and more effectively identify what is driving it. Most commonly, the patient will give a description of their pain with a wave of their hand over the area involved. This is not overly helpful and can be rectified by getting them to draw their pain on a diagram (see Pain Key). Directing them with a pain key is more useful than just asking them to draw, which generally ends up with random ticks, crosses and scribbles everywhere. If the patient has broad/achy pain or soreness, ask them to scribble, if it is sharp ask for a zigzag and if they have pins and needles, to draw dots.
Once this is done you need to work out where the majority of the pain is. Ask the patient to point with one finger to the majority of the pain (Fortin et al, 1997). For patients with focal pain they will generally use a single finger, with non-focal pain they will use three fingers or wave their hand around.
Key questions then are:
- “For the area of pain you are pointing at, how big is it? Golf ball, tennis ball, mango, football or larger?”
If it is a golf or tennis ball you are on a winner, as focal pain is generally easy to find. With mangos, footballs or bigger you need a little work to try shrink them down first, which we will come to under sensitisation.
Now you need to know how much of their pain is in the golf ball. While pointing at the pain diagram with the patient ask:
- “If that is the majority of the pain, how much of your pain is located in the golf ball? Is it 40, 50, 60, 70, 80, 90%?”
Commonly the patient will have coloured in a large area of the pain diagram and will say 90% of their pain is in the golf ball. This is always a relief as you can then focus on sorting the pain in the golf ball and see what is left at a later date.
You have now sorted where the majority of the pain is. To finish their ‘Mapping their Pain’ you need to clarify how bad it is. This is done easily with four quick questions.
- “If 10 is the worst pain you can imagine and 0 is nothing, what is your pain at its worst?” Answer 9/10.
- “How often is it 9/10? Once a day, week, month. Multiple times a day?” The answer is always “It depends what I do”. Which is logical, but you just want to get an idea how often they are in significant pain, so try get it down to how many times per day or week.
- “When it is not 9/10, what is it on average?”
- “How often is it 0/10?” This will vary from “never” to “most of the week”. Clearly this changes your treatment approach
Very quickly you have a good feel for the patient’s location and severity of pain, and whether they are sensitised. Next you need to tease out the remaining features of their pain.
Inflammatory features are as they were in medical school. Worse in the morning and after rest, associated with stiffness and swelling, improved with heat, worse with cold and commonly transiently respond to anti-inflammatories. Bony features are a little more difficult to define. This is pain on impact and palpation over bone, and commonly result in night pain that wakes the patient. Myofacial features are muscle tightness, trigger points or cramping, and the patient commonly reports improvement with massage, acupuncture or manipulation that lasts about 1-3 days. Mechanical features include instability, locking, decreased ROM, and painful clicking and clunking. Finally, ischaemic features are the standard claudicant-type pain.
Aggravating and relieving factors help add layers to the picture and better define the structures that may be responsible for the pain. That completes the nociceptive pain. The next tasks are to determine whether they have neuropathic pain or are sensitised.
Neuropathic pain is defined as pain due to nerve damage (Baron et al, 2010). However, patients commonly present with features of neuropathic pain with no nerve damage. These features include burning, pins and needles, numbness, electric shocks, and crawling (formication). An answer of “yes” when asking about these sensations can be a light bulb moment in the consult, as neuropathic features or pain is commonly associated with a worse pain and the patient being emotionally distressed (Koop et al, 2015).
‘Sensitisation’
The next question to answer is, “Is the patient sensitised?”. Sensitisation can be thought of as the pain being greater than the injury, and explained to the patient as “Sensitisation can be thought of as the ‘volume control’ for your pain. Commonly, pain is ‘turned down’, particularly from degenerative problems, which normally don’t cause pain. But changes occur resulting in the volume being ‘turned up’, and things that shouldn’t hurt, do hurt, and things that should only hurt a little bit, hurt a lot.”
By the time you are this far into the history you will have a good feel as to whether the patient is sensitised or not. Key indicators are: severe pain, pain that has lasted a long time, pain with no trigger, a pain diagram with large areas coloured in, the patient being emotionally distressed, changes in pain with stress or holidays and pain that does not make sense. “If you are confused, they are sensitised”. Clearly, with disconcordant pain you need to be thinking about malignancy and inflammatory disorders. However, with a patient who describes pain that starts at their buttocks, shoots up their back, and wraps around their right eye (yes a real patient), it is unlikely to be a tumour – but they are very likely to be sensitised. There are also a number of risk factors for sensitisation including multiple allergies, food intolerances, irritable bowel syndrome, chronic fatigue, fibromyalgia, migraines, anxiety, depression and temporomandibular syndrome. These are linked to central sensitisation syndrome and commonly associated with chronic pain (Nijs et al, 2010).
Quickly tick off your red flags (any history of fevers, shivers, shakes, night sweats or pain, significant recent weight loss without trying, past or current cancer). Then find out what they have already done for their pain. Here you need to get a feel for compliance with previous treatments and identify what they do and don’t want. Most notably, “I don’t take medications” and “I don’t want any injections and/or an operation”. In some ways this makes it easier, as the patient has shrunk down your treatment options, highlighted the things they are unlikely to be compliant with, and identified what probably won’t work, (since they don’t think it will!).
Finally, contributing factors usually come from the examination and include obesity, strength deficits, limitations in ROM, biomechanical abnormalities such as knee varus or valgus and pes planus.
A patient with lower back pain could be summarised as having “Somatic referred lower back pain with inflammatory, myofascial and neuropathic features. This is in the setting of obesity, poor gluteal strength and a moderate degree of sensitisation.” The differentials for the origin of the pain can then be defined.
Each one of above features provide you with treatment options and, once identified, are used to define your treatment plan.
Summary
The patient’s pain map, features of pain and previous treatment, in combination with your experience, will allow you to tailor a simple but targeted and comprehensive treatment strategy. Once you have started sorting out the patient’s pain you can then move on to introducing exercise (Rule of 2’s), and then weight loss (4H’s). We will cover these in the following issues.
References:
Baron R, Binder A, Wasner G. Neuropathic pain: diagnosis, pathophysiological mechanisms, and treatment. Lancet Neurol. 2010 Aug;9(8):807–19.
Fortin JD, Falco FJ. The Fortin finger test: an indicator of sacroiliac pain. Am J Orthop. 1997 Jul;26(7):477–80.
Koop SMW, Klooster PM Ten, Vonkeman HE, Steunebrink LMM, van de Laar MAFJ. Neuropathic-like pain features and cross-sectional associations in rheumatoid arthritis. Arthritis Res Ther. 2015 Sep 3;17(1):237.
Nijs J, Van Houdenhove B, Oostendorp RAB. Recognition of central sensitization in patients with musculoskeletal pain: Application of pain neurophysiology in manual therapy practice. Man Ther. 2010 Apr;15(2):135–41.