A US survey has found health inspections and other quality ratings aren't nearly as important as better staff ratios when it comes to controlling infections in nursing homes.
Welcome to The Medical Republic‘s COVID Catch-Up.
It’s the day’s COVID-19 news into one convenient post. Bianca is away until tomorrow – till then please email penny@medicalrepublic.com.au. with any tips, comments or feedback.
10 August
- Staff numbers predict COVID in aged care
- US health insurers profiting from the pandemic
- Guess who won’t get vaccinated
- World hits 20 million cases
- Pasteurising breast milk kills SARS-CoV-2
-
- The pandemic has brought the quality of aged care into excruciatingly sharp focus – especially in Australia, where nursing homes have accounted for more than half of deaths. A study in JAMA of nursing homes in eight US states has looked for correlations between various quality ratings and number of COVID-19 cases. Interestingly, the researchers found staffing levels were the only good predictor: homes with more staff per resident had fewer cases, while better ratings on health inspections or other quality measures made no difference. “These findings suggest that poorly resourced [nursing homes] with nurse staffing shortages may be more susceptible to the spread of COVID-19,” the authors write. “Although guidance on best practices on infection control are important… policies that provide immediate staffing support may be more effective at mitigating the spread of COVID-19.”
This comes just after a record day of 14 deaths in Australian aged care, and as our Royal Commission into Aged Care has heard that the government made no COVID-19 plan for the sector and failed to investigate early outbreaks. - Think the pandemic is bad for business? You’re clearly not a large American health insurer. According to an analysis of the latest quarterly reports by Statista, some of the major players, such as UnitedHealth Group, Anthem and Humana, have doubled their multi-billion-dollar quarterly profits through not having to pay out for major surgeries and other procedures. This is despite the Affordable Care Act requiring insurers to pay out rebates and capping their profits. The US health department has reportedly taken a dim view and advised them to reduce their premiums.
- In more face-smacking news out of the US, a Gallup poll has found that more than a third of Americans would not get a COVID vaccine even if it was FDA-approved and available free. As we’ve come to expect, this divides along partisan lines: while 65% of respondents overall said “yes please” to the hypothetical vaccine, among Democrat respondents the figure was 81% and among Republicans only 47%. Younger people (18-29) were more likely to tick “gimme” than middle-aged folks (50-64) – 76% to 59% – but the proportion went up again (70%) in the over-65s.
Reassuringly, a letter in The Lancet at the end of June reported a survey of Australians back in April which found only 4.9% would not get a vaccine. - That COVID-19 counter from Johns Hopkins that we’ve all been watching since cases were in the mere tens of thousands has now ticked past 20 million. It’s taken about six weeks, since June 28, to double from 10 million.
It’s widely believed that the true numbers are well above what’s reported, thanks to the high proportion of asymptomatic cases that continues to puzzle COVID-watchers. And this has led to some interesting speculation about whether the novelty of the novel coronavirus may have been exaggerated: were humans as universally susceptible to it as we’ve assumed, or were some of us already carrying some partial immunity from previous exposures to other coronaviruses? - In some good news, a study from the University of NSW has found that pasteurising breast milk inactivates SARS-CoV-2, though the same can’t be said for cold storage. The team experimentally infected small amounts of expressed breast milk from healthy donors and heated it to 63?C for 30 minutes, after which no infectious live virus remained. It’s only a theoretical risk that infectious virus – as opposed to detectable RNA – could be passed on via donor breast milk, such as that from the milk banks that feed vulnerable babies around the world. But as lead author Greg Walker, a PhD candidate in Professor Bill Rawlinson’s group at UNSW Medicine, said: “We’ve seen in previous pandemics that pasteurised donor human milk supplies may be interrupted because of safety considerations, so that’s why we wanted to show that [it] remains safe.”
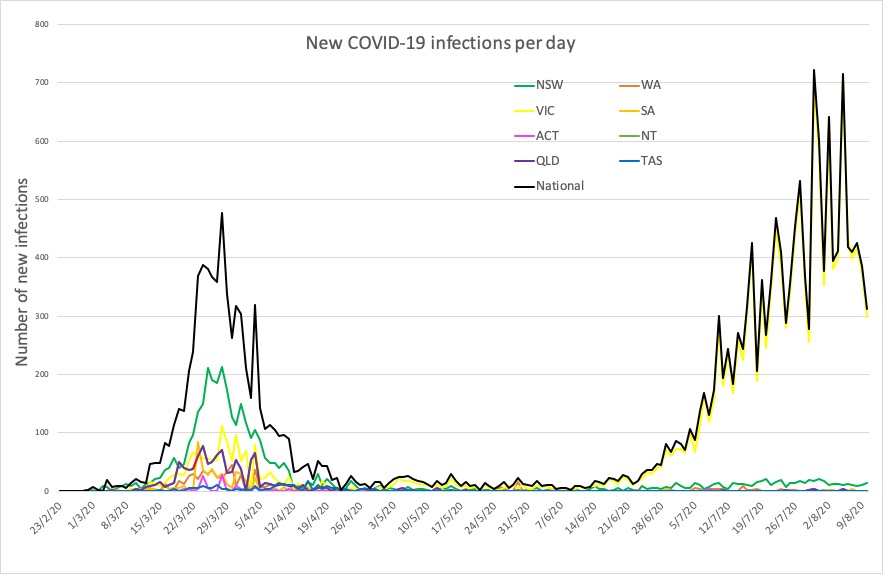
- Here are the confirmed COVID-19 infection numbers from around Australia to 9pm Monday:
National – 21,397, with 313 deaths and 664 hospitalised
ACT – 113
NSW – 3875
NT – 33
QLD – 1089
SA – 459
TAS – 229
VIC – 14,957
WA – 642
- The pandemic has brought the quality of aged care into excruciatingly sharp focus – especially in Australia, where nursing homes have accounted for more than half of deaths. A study in JAMA of nursing homes in eight US states has looked for correlations between various quality ratings and number of COVID-19 cases. Interestingly, the researchers found staffing levels were the only good predictor: homes with more staff per resident had fewer cases, while better ratings on health inspections or other quality measures made no difference. “These findings suggest that poorly resourced [nursing homes] with nurse staffing shortages may be more susceptible to the spread of COVID-19,” the authors write. “Although guidance on best practices on infection control are important… policies that provide immediate staffing support may be more effective at mitigating the spread of COVID-19.”