Raising the possibility of adenomyosis as an underlying cause of a woman’s heavy menstrual bleeding can be critical
What is adenomyosis?
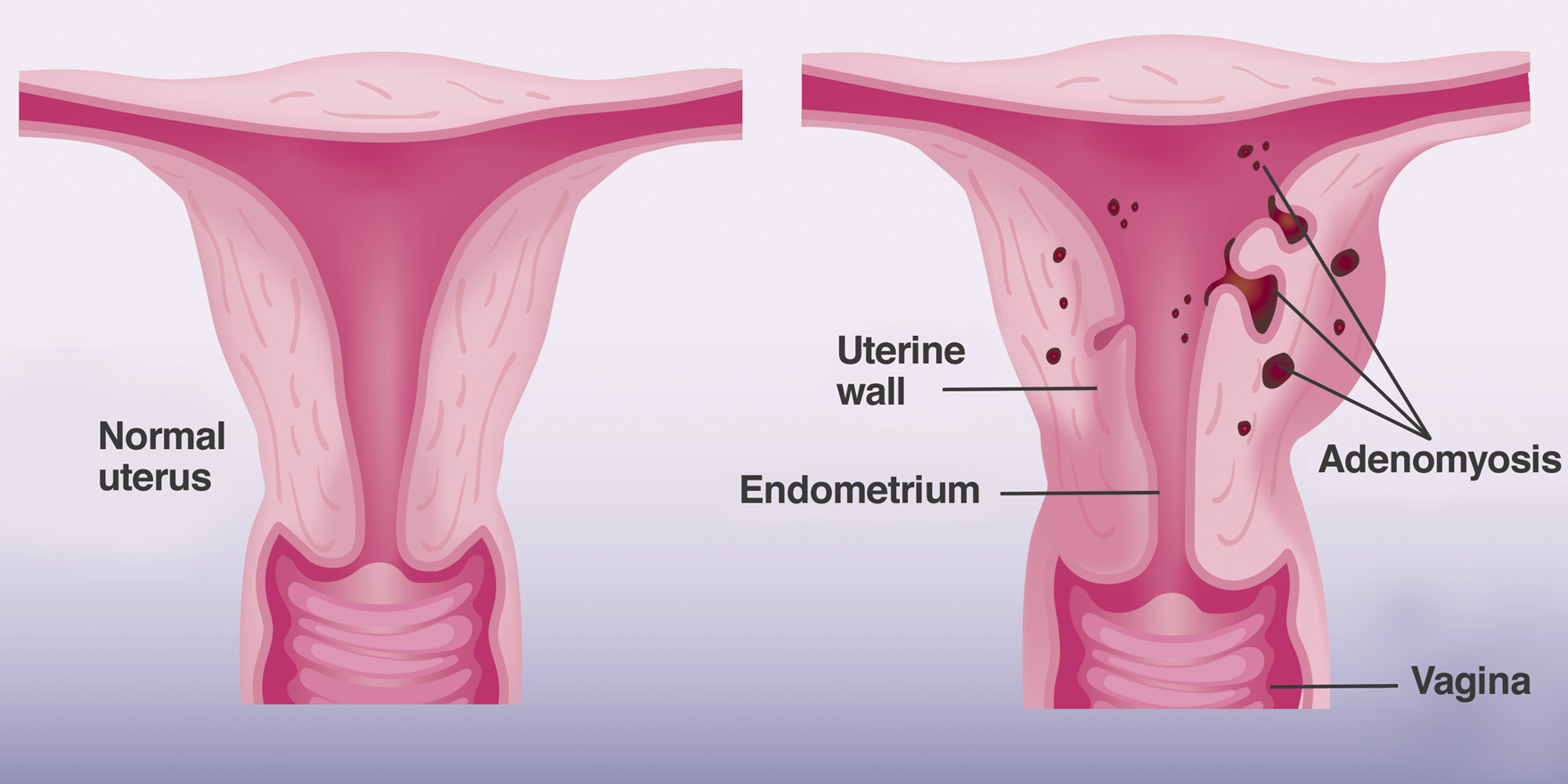
Like endometriosis, adenomyosis is due to the presence of ectopic endometrial tissue, located within the uterine muscle wall.
Not only may women suffer from severe period pain, they may also have heavy menstrual bleeding.
The uterus can be enlarged due to reactive myometrial hyperplasia and hypertrophy. Adenomyosis can be found in up to 70% of hysterectomy specimens, and therefore may be far more common than appreciated clinically.1
What are the causes?
Previous trauma may cause endometrial invagination into the myometrium. Multiparity, termination of pregnancy, uterine curettage and caesarean section are risk factors.2
As an oestrogen dependent pathology, women’s age, early menarche, short menstrual cycles, obesity and tamoxifen use are also risk factors. There is also association between adenomyosis, depression and use of antidepressant medication.3
How do we diagnose?
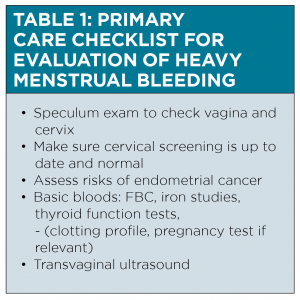
Clinical suspicion is the key to diagnosis. Women with adenomyosis typically complain of heavy menstrual bleeding and severe period pain. The uterus can be enlarged and tender.
Sonographers may need to be alerted on the ultrasound request form to look for the subtle signs of adenomyosis on transvaginal ultrasound.

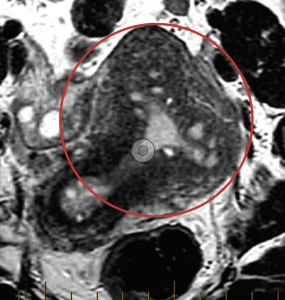
MRI is more accurate than transvaginal ultrasound, especially when the adenomyosis is superficial or diffuse, and when coexisting fibroids maybe confused with focal adenomyosis.
What can we do as GPs?
GPs can play a pivotal role in the diagnosis and early management of adenomyosis.
The most important role is to raise the possibility of adenomyosis as the potential underlying cause of a woman’s heavy menstrual bleeding and severe period pain. When requesting transvaginal ultrasound, possibility of adenomyosis should be communicated to alert sonographers to look for the subtle signs.
GPs may initiate medical therapies such as tranexamic acid, NSAIDs, progestins or a low-dose continuous combined oral contraceptive pills (COCP) as first line treatment for symptomatic control.4.5
Although most of these treatments have not been tested specifically for adenomyosis6,7, they are still recommended in the current Australian Clinical Care Standard for the symptomatic management of heavy menstrual bleeding.6
How about combined oral contraceptive pills?
Low-dose, continuous combined oral contraceptive pills (COCP) with withdrawal bleeds every four to six months can be effective in relieving heavy menstrual bleeding and dysmenorrhoea.8 There are, however, no well-conducted RCTs available to support their use in adenomyosis. More than 30 COCP registered brands are available in Australia. A guide is available to help GPs to choose the right one for their patients.9
Go to this link to learn more:
https://www.nps.org.au/australian-prescriber/articles/choosing-a-combined-oral-contraceptive-pill
How good are progesterone-releasing IUDs?
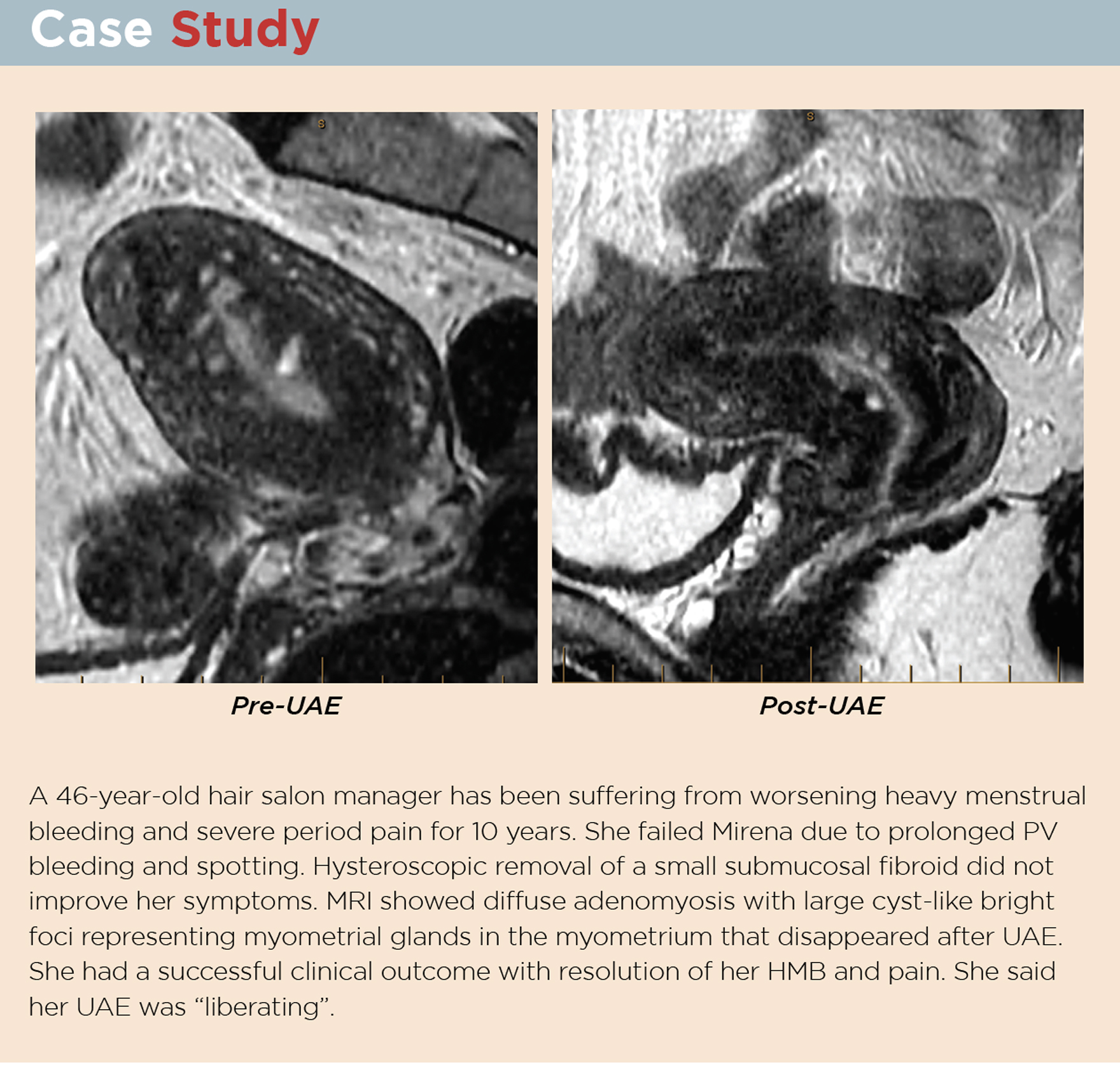
The Levonorgestrel Intrauterine Drug Delivery System (LNG-IUS) (Mirena; Bayer Australia Ltd) releases 20 mcg levonorgestrel daily for up to five years. This is currently the best-evaluated and the most efficacious non-surgical treatment for adenomyosis.10,11
An RCT from Turkey comparing LNG-IUS and hysterectomy showed comparable increase in haemoglobin and similar QoL scores.12
A three-year study from China showed a significant drop in pain score in patients treated with Mirena. Patient satisfaction rate was only 56.3% at 12 months, however.
Prolonged light bleeding (25%) or irregular bleeding (14%), and other side effects such as weight gain, ovarian cyst formation, lower abdominal pain and acne contributed to the less than ideal satisfaction rate.13
More recent studies have shown LNG-IUS to be less effective in women with extensive adenomyosis, or with a uterine volume larger than 150ml. A discontinuation rate of 70% is noted in women with uterine volume larger than 314ml.14
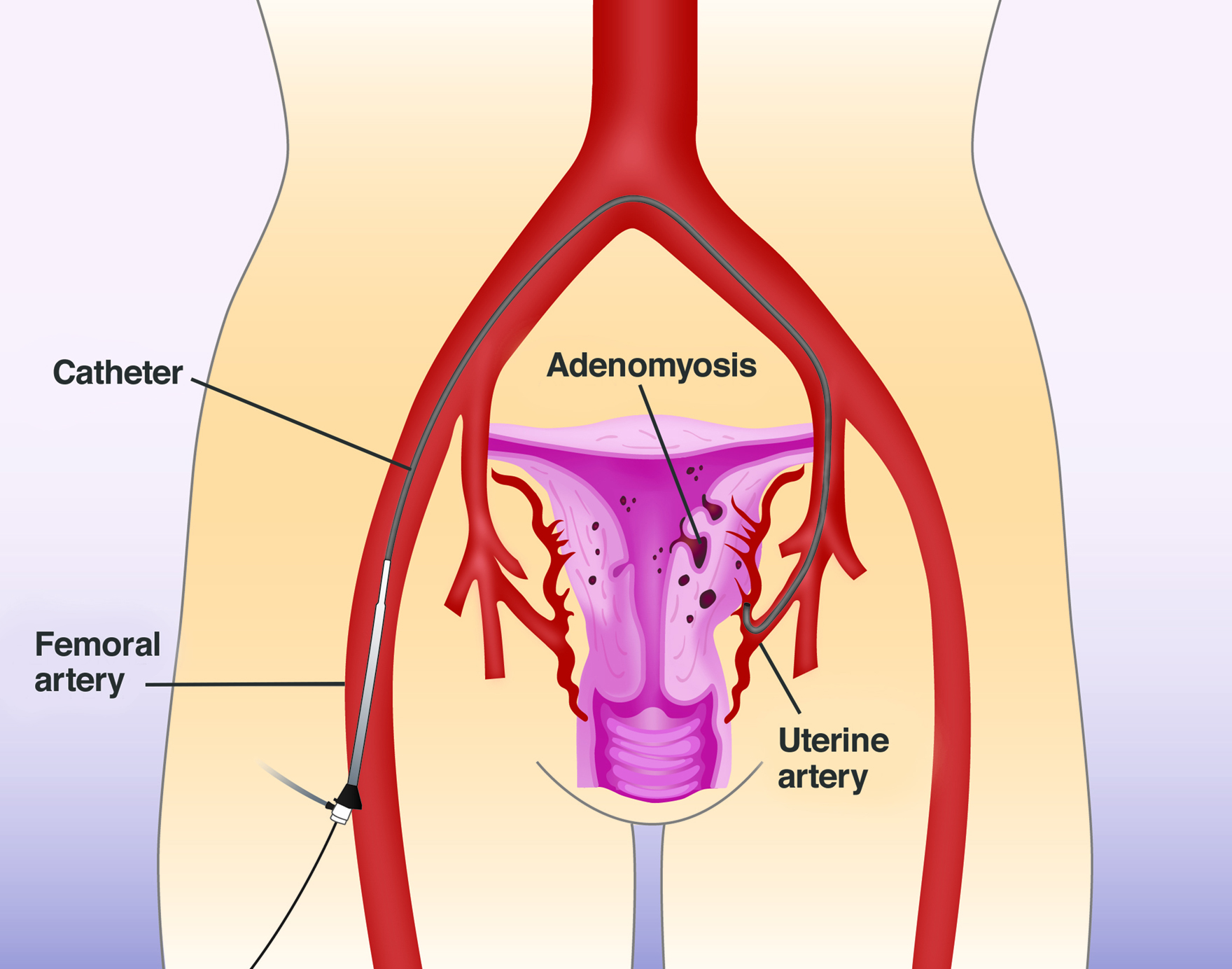
What is UAE? How does UAE work?
Uterine Artery Embolisation (UAE) is an interventional radiology procedure that can be performed under local anaesthetic and light conscious sedation. It requires usually only a one-night hospital stay and one-week recovery.
During UAE, an angiographic catheter is used to selectively cannulate each of the two uterine arteries. Embolic particles are then suspended in contrast medium and injected into the uterine arteries to induce ischaemia. Normal uterine myometrium has many dormant arteries that are normally shut down. It has an immense capacity to recruit dormant arteries to survive the ischaemic insult. The adenomyotic tissue, however, has no capacity to do this. Its sole blood supply is therefore vulnerable to being blocked by embolic particles.
Because pathologic lesions like adenomyosis or fibroids do not have the capacity to recruit new vessels they will therefore suffer irreversible ischaemic infarction if their blood supply is embolised.
Watch the video:
“How does UAE work for adenomyosis”
https://www.youtube.com/watch?v=vP9XsxF0T5w
How safe and effective is UAE?
UAE has been performed to treat fibroids since 1995 and now there have been seven RCTs comparing UAE and hysterectomy for fibroid treatment, resulting in a Cochrane Review in 2014 confirming the safety and effectiveness of UAE for fibroids.15
There are no RCTs comparing UAE and hysterectomy in the setting of adenomyosis. However, a meta-analysis in 2018 consists of 30 studies including 1049 adenomyotic women treated with UAE and confirms safety and effectiveness.16
Our local Australian study published in 2008 is one of the largest ever performed, treating 117 women with severely symptomatic adenomyosis using UAE. Overall clinical success was achieved in 89% of women. Heavy menstrual bleeding was successfully controlled in 88% of women. It is highly effective for dysmenorrhoea, with significant VAS pain score reduction (from 7.45 to 1.32). There were no major complications. Only 5% of women had hysterectomy due to unsatisfactory symptom relief. 17
Can women still get pregnant after UAE?
Successful term pregnancies following UAE for the treatment of fibroids have been reported in many case series.
For adenomyotic women, however, there is currently insufficient data on the impact of UAE on fertility and pregnancy.16,17 Following UAE for adenomyosis, there is more than a 90% chance that the uterus can be retained, but it remains unclear if UAE will positively or negatively affect fertility and pregnancy.
Study has shown that GnRHa before IVF improved the pregnancy rate.18 For adenomyotic women seeking pregnancy, GnRHa treatment could be an option for women seeking symptom control and immediate fertility.
Should endometrial ablation be used for adenomyosis?
Endometrial ablation uses heat energy to destroy endometrial lining and treats only acfew millimeters depth of tissue. Studies have shown an increased failure rate for ablation treatment of adenomyosis invading deeper than 2.5mm. If the diagnosis were made on MRI, the depth of involvement would have to be more than 8mm to meet diagnostic criteria.
Clearly, ablation is unlikely to achieve this depth. Sealing off the endometrial glands may even worsen dysmenorrhoea.19,20
Even with more recent technology (Novasure), adenomyosisis found to be a risk factor for failure of endometrial ablation, resulting in a higher rate of subsequent hysterectomy.21
|
Table 2: medical therapy for heavy menstrual bleeding in general practice |
|
|
Tranexamic Acid |
Action: Antifibrinolytic |
|
NSAID: Mefenamic Acid |
Action: Inhibits prostaglandin synthesis |
|
Combined Oral Contraceptive Pills (COCP) |
Action: Stabilise lining of uterus, suppress cyclical hormone changes, prevent mid cycle oestrogen surge. |
|
Progesterone-releasing IUD |
Action: endometrial atrophy |
*CI: contraindications; SE: side effects.
Can adenomyosis be surgically resected?
Focal adenomyosis or adenomyoma can simulate fibroids on transvaginal ultrasound. Surgical resections have been attempted with the incorrect pre-operative diagnosis. Unlike fibroids, the boundary between adenomyosis and the adjacent myometrium is anatomically indistinct and therefore adenomyotic tissue cannot be enucleated.
Uterine-sparing surgery should not be undertaken lightly for adenomyosis.22
Many cases of adenomyosis are seen involving an infiltrative lesion diffusely affecting large areas of uterus, and therefore complete resection is not possible.
Is ‘wait for menopause’ a good wisdom still?
Adenomyosis is an oestrogen dependent condition and will become worse during the perimenopause time. Periods remain heavy and painful, and the situation could be worse with added cycle unpredictability. If a woman requires hormone replacement therapy, the oestrogen component might worsen adenomyosis.
Is hysterectomy still ‘the only solution’ in the 21st century?
In the past, hysterectomy was seen as the only definitive treatment for women suffering from adenomyosis related symptoms. From early 2000, reports have emerged documenting the effectiveness UAE as an effective non-surgical alternative to hysterectomy.
How does adenomyosis affect fertility?
Adenomyosis has a negative impact on fertility and pregnancy.22
Women with adenomyosis are more likely to have premature delivery or premature rupture of membranes.23
Adenomyosis can also have a detrimental effect on IVF outcomes, reducing pregnancy rate and live birth rate.24
How is adenomyosis related to endometriosis?
Unlike adenomyosis, endometriosis is due to ectopic endometrial tissue outside the uterus – anywhere else in the abdomen and pelvis.
There is strong association of the two disease processes in 80 to 90% of cases.25
If a woman is suffering from both heavy menstrual bleeding and dysmenorrhoea, then the treatment should be aimed at adenomyosis. If the only symptom is dysmenorrhoea and medical imaging is negative for adenomyosis, then the focus should be on possible endometriosis.
Summary
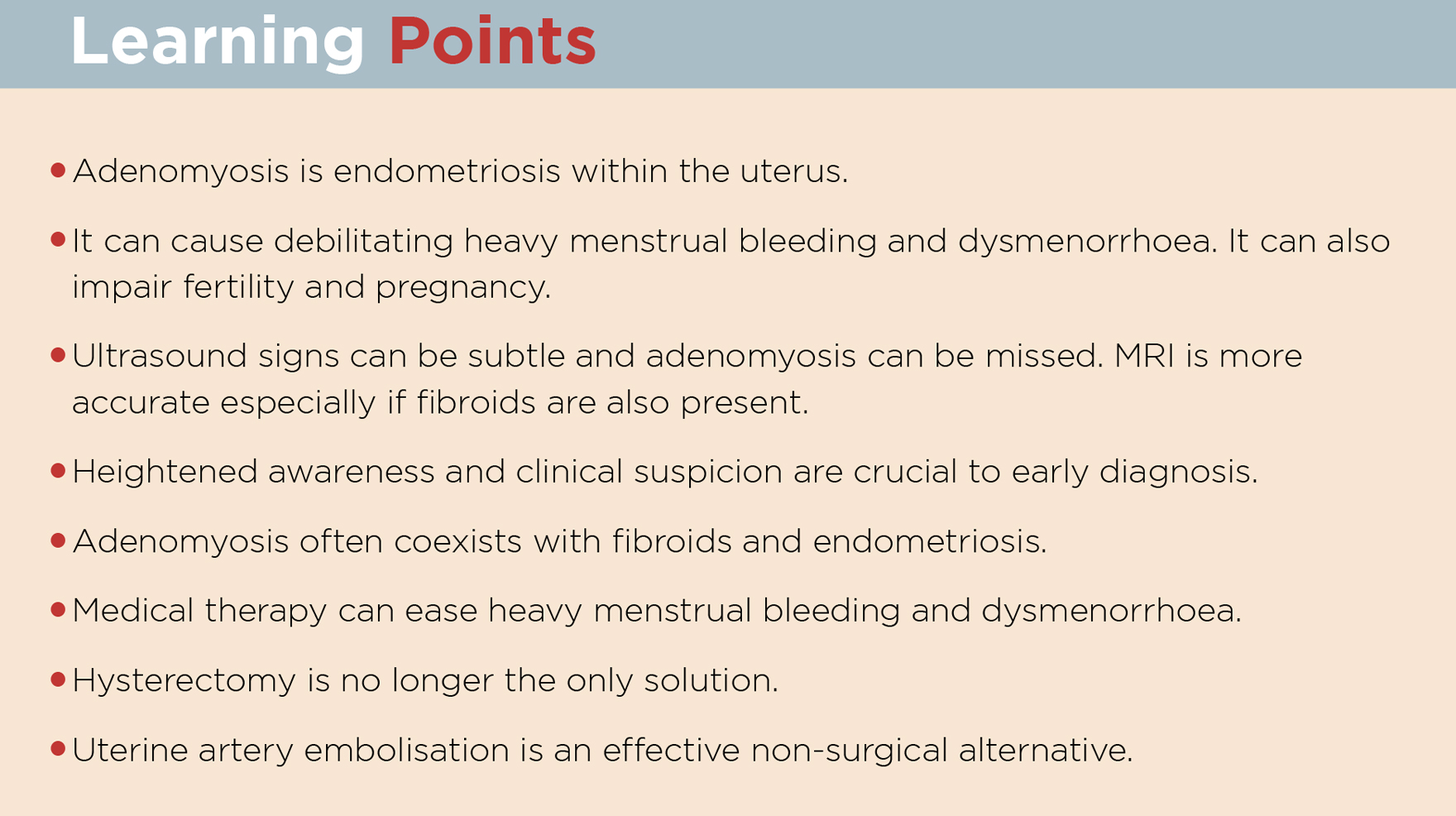
Adenomyosis is a common, but under-recognised pathology. It can produce debilitating heavy menstrual bleeding and dysmenorrhoea.
Treatment is available through a range of medical and surgical options, including uterine artery embolisation as an alternative to hysterectomy.
Consideration should be given to all modalities of treatment depending on a woman’s wishes and the nature of her symptomatology. For this to occur, adenomyosis must be recognised on clinical history, diagnosed with appropriate imaging, and treated in a woman-centred context.
All images copyrighted to Dr Eisen Liang
Dr Eisen Liang is an interventional Radiologist and Dr Bevan Brown is an obstetrician gynaecologist. Together they have collaborated for more than 10 years and founded Sydney Fibroid Clinic to help women to resolve fibroid and adenomyosis related symptoms, using minimally invasive procedures to achieve uterine conservation. Their research papers on fibroid disease and adenomyosis have been presented internationally and published in ANZJOG. For further information, please visit
www.sydneyfibroidclinic.com.au
References
- Mehasseb MK HM. Adenomyosis Uteri: an update. (2009). The Obstetrician & Gynaecologist 11: 41-47
- Pathophysiology of adenomyosis. Ferenczy A. Hum Reprod Update. 1998;4(4):312.
- Fertil Steril. 2010 Sep; 94(4): 1223–1228. Understanding adenomyosis: a case control study F. Andrei Taran, M.D.,Amy L. Weaver, M.S.,Charles C. Coddington, M.D., and Elizabeth A. Stewart, M.D.
- Medical management of heavy menstrual bleeding, Jacqueline A Maybin, Hilary OD Critchley, Women’s Health (2016) 12(1), 27–34
- Available management options for heavy menstrual bleeding, Prescriber ,19 September 2014
- Mehasseb MK HM. Adenomyosis Uteri: an update. (2009). The Obstetrician & Gynaecologist 11: 41-47
- Azziz R. Adenomyosis: current perspectives. Obstet Gynecol Clin North Am 1989; 16:221–35.
- Moghissi KS. Treatment of endometriosis with estrogen-progestin combination and progestogens alone. Clin Obstet Gynecol 1988; 31:823–8.
- Choosing a combined oral contraceptive pill. Mary Stewart and Kirsten Black Australian Prescriber 2015; 38:6-111 Feb 2015
- Streuli I, Dubuisson J, Santulli P et al. An update on the pharmacological management of adenomyosis Expert Opinion on Pharmacotherapy, 11/2014, Volume15, Issue 16
- Struble, Jennifer; Reid, Shannon; Bedaiwy, Mohamed A. “Adenomyosis: A Clinical Review of a Challenging Gynecologic Condition”. Journal of Minimally Invasive Gynecology. 2016 23 (2): 164–185.
- Ozdegirmenci O, Kayikcioglu F, Akgul MA, et al. Comparison of levonorgestrel intrauterine system versus hysterectomy on efficacy and quality of life in patients with adenomyosis. Fertil Steril 2011;95(2):497-502
- Sheng, J, Zhang, J P, Zhang, W Y et al. The LNG-IUS study on adenomyosis: a 3-year follow-up study on the efficacy and side effects of the use of levonorgestrel intrauterine system for the treatment of dysmenorrhea associated with adenomyosis Contraception, 2009, Volume 79, Issue 3
- Relationship between uterine volume and discontinuation of treatment with levonorgestrel-releasing intrauterine devices in patients with adenomyosis. Lee, Ki Hwan; Kim, Jang Kew; Lee, Min A; Ko, Young Bok; Yang, Jung Bo; Kang, Byung Hun; Yoo, Heon Jong Archives of Gynecology and Obstetrics, 2016, Vol.294(3), p.561(6)
- Gupta JK, Sinha A, Lumsden M, Hickey M. Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database Syst Rev. 2014 CD005073.
- Uterine Artery Embolization for the Treatment of Adenomyosis: A Systematic Review and Meta-Analysis, de Bruijn, Annefleur M.; Smink, Marieke ; Lohle, Paul N.M. ; Huirne, Judith A.F. ; Twisk, Jos W.R. ; Wong, Caroline ; Schoonmade, Linda ; Hehenkamp, Wouter J.K. , Journal of Vascular and Interventional Radiology, December 2017, Vol.28(12), pp.1629-1642.
- A Clinical audit on the efficacy and safety of uterine artery embolisation for symptomatic adenomyosis: Results in 117 women, Liang, Eisen; Brown, Bevan; Rachinsky, Maxim Australian and New Zealand Journal of Obstetrics and Gynaecology, August 2018, Vol.58(4), pp.454-459
- Grace Younes, Togas Tulandi Effects of adenomyosis on in vitro fertilization treatment outcomes: a meta-analysis Fertility and Sterility, Volume 108, Issue 3, September 2017, Pages 483-490.3
- McCausland AM, McCausland VM. Depth of endometrial penetration in adenomyosis helps determine outcome of rollerball ablation. Am J Obstet Gynecol 1996;174:1786–93; 1793–4.
- The response of adenomyosis to endometrial ablation/resection. McCausland V, McCausland A Hum Reprod Update. 1998;4(4):350.
- Effect of Undiagnosed Deep Adenomyosis After Failed Novasure Endometrial Ablation Mengerink, Bianca B.; van Der Wurff, Anneke A.M.; Ter Haar, Johanne F.; van Rooij, Ilse A.; Pijnenborg, Johanna M.A. The Journal of Minimally Invasive Gynecology, February 2015, Vol.22(2), pp.239-244
- J.A. Abbott. Adenomyosis and Abnormal Uterine Bleeding (AUB-A) -Pathogenesis, diagnosis, and management Best Practice & Research Clinical Obstetrics and Gynaecology 40 (2017) 68-81
- Juang CM, Chou P, Yen MS, et al. Adenomyosis and risk of preterm delivery. BJOG 2007;114(2):165-9.
- Effect of a sonographically diffusely enlarged uterus without distinct uterine masses on the outcome of in vitro fertilization-embryo transfer. Chiang CH, Chang MY, Shiau CS, Hou HC, Hsieh TT, Soong YK J Assist Reprod Genet. 1999 Aug; 16(7):369-72.
- Leyendecker G, Bilgicyildirim A, Inacker M, et al. Adenomyosis and endometriosis. Re-visiting their association and further insights into the mechanisms of auto-traumatization. An MRI study. Arch Gynecol Obstet 2015;291(4):917-32.