Every dollar invested into social prescribing returns $4.43 to society through improved wellbeing and reduced costs to the health system.
Social prescribing returns investment four times over, finds Canadian study.
As described by the RACGP, social prescribing is “a means of enabling GPs, nurses and other primary care professionals to refer people to a range of local, non-clinical services”.
Speaking at the Australia Medical Students Association Global Health Conference, South Australia-based GP Dr Patrick Daly said it was important for GPs to take social determinants of health – like education level, availability of open spaces – into account when incorporating social prescribing into their practice.
“Social prescribing is something we’ve always done in primary care, and it has a very natural primary-care focus, because primary care sits in the community,” he told delegates.
“I think the way I describe social prescribing is that it’s an umbrella term that encapsulates lots of different things… it’s a pathway as well as being a physical bit of advice.”
Despite the RACGP touting the benefits of social prescribing in 2019, systemic adoption in a more organised form has been slow.
Related
But not without reason, said Dr Daly.
“The reason why we have to be careful with social prescribing, the reason why it’s getting off the ground in the way it is, which can sometimes feel very slow, is because we have to avoid the mistakes of the past,” he said.
“We have to avoid doing things just because we think it’s a good idea.
“We have to have an evidence base for it, we have to structure it properly, resource it properly, because we don’t want to be snake oil salesmen.”
At Dr Daly’s practice north of Adelaide, a link worker or community navigator, connects the health system to the wider web of social services.
“You’ve got this interface between the roots of the community and the services, [but] how do we get there? The trunk of the tree is the link worker,” he said.
“It’s very primary care focused, but it’s hugely relevant to secondary care as well.”
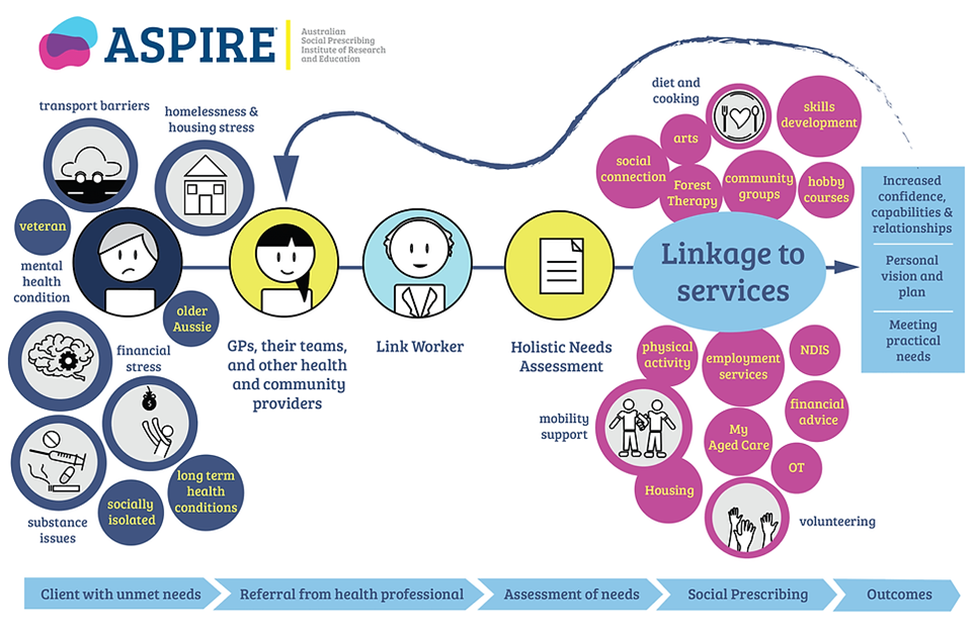
Source: ASPIRE
Beyond improving wellbeing – particularly measures like loneliness – social prescribing, like general practice, offers bang for buck.
Earlier this year, the Canadian Institute for Social Prescribing commissioned KPMG to undertake an analysis of the economic return on social prescribing projects.
The analysis found a return of CAD$4.43 per dollar invested and better health outcomes – namely increased wellbeing and reduction in healthcare utilisation – particularly for older adults and youth.
In aging adults, social prescribing resulted total savings of CAD$268 million per year and improved quality of life by supporting aging at home and reducing hospital utilisation.
An additional CAD$59 million in employment income per year was generated through social prescribing, particularly among the youth.
“Diving deep into these areas where robust public evidence exists, the analysis is clear: social prescribing is an impactful tool in the toolbox to improve the health and wellbeing of Canadians,” the analysis found.
“And when social prescribing and communities are appropriately resourced, we can expect to see reductions in unnecessary health service utilisation, and significant long-term cost savings.”
Dr Daly encouraged delegates to ask practices they were involved with to become “parkrun practices”, an initiative orchestrated through the RACGP which allows GPs to “prescribe” the free, socially-focused, family-friendly 5-kilometre parkrun events to their patients.
The Australia Medical Students Association Global Health Conference 2024 took place 20-23 September at the National Wine Centre in Adelaide.





