Without appropriate treatment, the seroma persists and may result in superimposed infection.
This 62-year-old male originally presented in 2014 with ongoing swelling over the left upper thigh and pelvis following a cycling accident that involved direct trauma to this region at speed.
During the high-speed injury, the patient landed on the left side of his pelvis.
On examination, there was a fluctuant subcutaneous collection that was not particularly painful over the site of trauma. This was further investigated with ultrasound and subsequently MRI.
There was an anechoic (that is, fluid contents, without debris) collection seen on ultrasound between the iliac crest and lateral thigh located at the junction of the subcutaneous tissues with the fascia of the fascia lata/iliotibial band. This was percutaneously aspirated twice but recurred.
Further investigation was performed with CT and MRI where there was a large fluid collection at the interface between the subcutaneous tissues and the superficial surface of the iliotibial band/fascia lata with a low signal capsule. This demonstrated low signal on T1 and high signal on T2, similar to that of water. The underlying iliotibial band was intact.
This collection persisted for years, and has been monitored with MRI.
The history and imaging characteristics would indicate a post-traumatic seroma, termed a Morel-Lavallee lesion. Typically this lesion is due to a closed degloving injury where a shear force is applied to the lateral thigh at speed, and results in abrupt separation of the subcutaneous layer from the underlying deep fascia. At this interface, there are perforating vessels that pierce the deep fascia which drain lymph or blood into the perifascial plane.
This is significant, as without appropriate treatment, the seroma/fluid collection persists and may result in superimposed infection. Conservative treatment also may be attempted. A simple percutaneous drainage may not be curative and typically is followed by repetitive recurrences. An alternative treatment is to drain the collection under ultrasound completely, followed by injection of a sclerosing agent such as doxycycline and compressive bandaging post-procedure.
Surgical excision may be required for persistent encapsulated collections, and for infected or necrotic lesions.
Fig A: Initial ultrasound showing an anechoic (purely fluid) collection over the lateral thigh in the subcutaneous layer overlying the fascia lata, which was drained
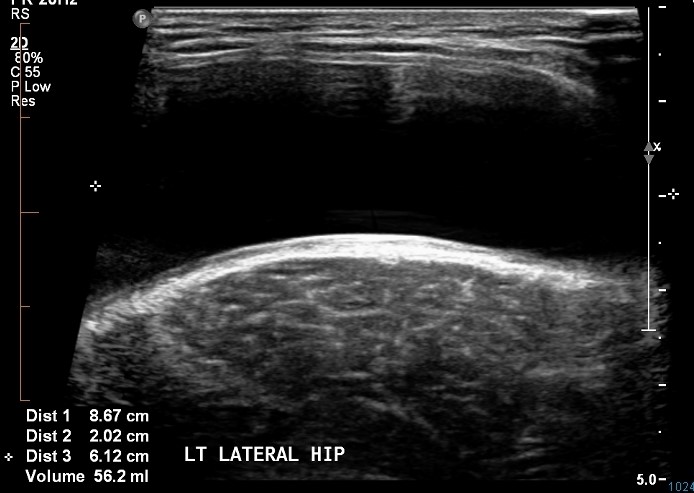
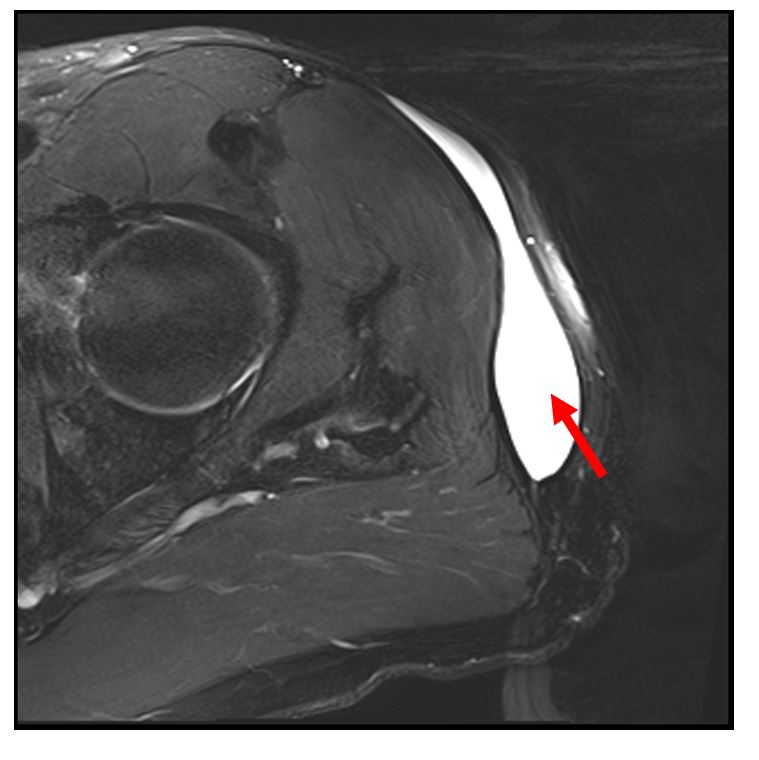
Fig B: Interval CT showing reaccumulation of fluid after percutaneous drainage (red arrow)

Fig C: Coronal PD MRI years later showing persistent fluid collection between the subcutaneous fat (green arrow) and the underlying fascia lata (blue arrows); the rim of low signal indicates encapsulation (red arrows)
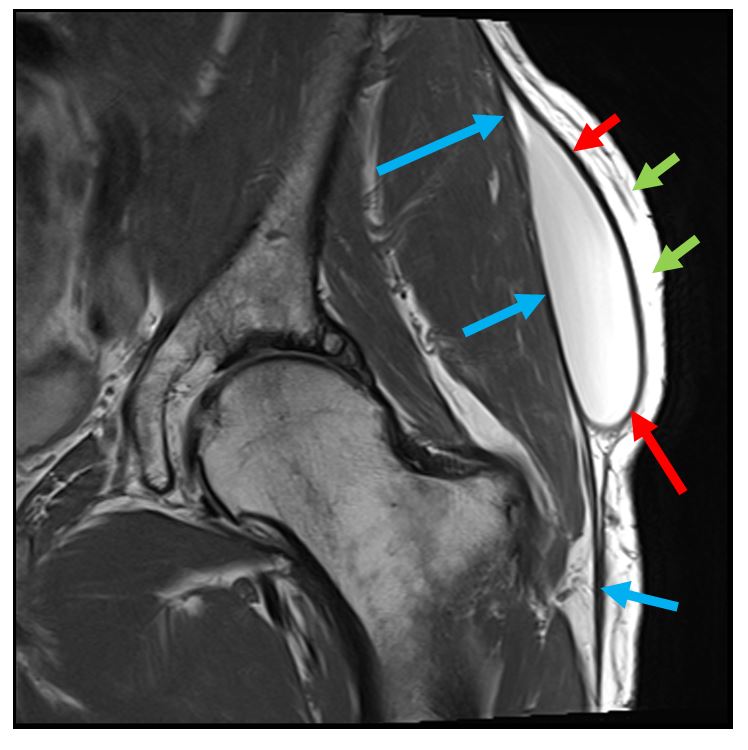
Fig D, E: Coronal and axial T2 fat saturated imaging showing fluid collection (red arrow)