Families can be anxious about therapy, often fearing blame. But in reality, clinicians understand most families are doing their best.
Half of all adult mental health issues emerge before the age of 14, with 14% of Australian children aged four to 17 currently impacted by poor mental health.
These are the drivers for the first National Children’s Mental Health and Well-being strategy, developed by the National Mental Health Commission and released by the government last week.
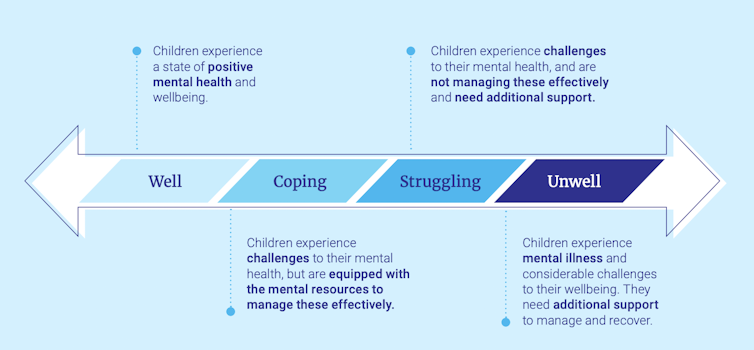
The strategy suggests viewing children’s mental health and well-being along a continuum of well–coping–struggling–unwell, and recommends focusing on support, prevention and early intervention before mental illness occurs.
The strategy also calls for “integrated child and family well-being services to better support families”. This means focusing on all the environments in which a child lives, learns and plays.
So what does the strategy recommend? And why is it important to get family involved in children’s mental health care?
Read more: Preventive measures are as important to the mental health pandemic as they are to COVID-19
Supporting the child’s family, school and community
The strategy recommends focusing on four key areas to improve Australian children’s mental health and well-being:
1. Empowering families to play a role.
This means having access to mental health information and education, and allowing parents to better identify the signs of poor mental health in their child. Families should be supported to access services in the community before their child becomes significantly unwell, potentially decreasing the need for more acute support.
2. Closing the gaps in access.
More than 50% of children with mental health issues are not receiving professional support, highlighting a significant gap in access. The strategy notes ways for services to better support families, including:
- improvements in system navigation so families can find the right help at the right time
- building the system to support children with complex care needs, for example, by providing support to engage with multiple government agencies
- upskilling the existing workforce to increase capacity.
3. Increasing the role for schools in supporting children’s well-being and mental health.
This includes:
- creating a culture within schools where well-being is nurtured
- providing targeted responses for at-risk youth
- supporting the development of educators that are trained and equipped to deliver well-being support.
While some of this work is already underway, the impacts of the COVID-19 pandemic, extended school absence and facial coverings on children cannot be underestimated.
4. Use treatments based on evidence.
Therapeutic treatments and supports should be based on scientific evidence from high quality research.
Why involve the family?
While therapies for children vary according to the issue of concern, more and more are integrating families at various stages to increase their effectiveness.
Guidelines for the treatment of oppositional defiant disorder and anorexia nervosa, for example, typically include either parent management training or family therapy, or both.
So how do they work? Let’s take a closer look at these examples.
Oppositional defiant disorder
Young people with oppositional defiant disorder display a frequent and persistent pattern of anger, irritability, arguing and defiance towards authority figures.
Read more: More than just a tantrum: here’s what to do if your child has oppositional defiant disorder
Parent management training for the disorder focuses on spending quality time with your child, providing positive reinforcement (such as praise) for desired behaviour and setting consistent limits for undesirable behaviour.
Family therapies vary, but typically ask all household members to attend sessions together. Discussion points may include understanding each family member’s views of the concern, identifying family strengths, exploring challenges and conflicts, encouraging consistency between parents and strengthening family bonds.
Research combined with our own clinical experience suggests including parents and/or family members in treatment results in better outcomes for children that are maintained longer, and typically in fewer sessions.
Anorexia nervosa
Family support is the gold standard in the treatment of anorexia nervosa and other eating disorders.
Anorexia nervosa is a psychological illness that results in low body weight and body image distortion. Young people with anorexia nervosa restrict the types and amount of food they eat and will often engage in extreme forms of weight loss, such as excessive exercise.
Read more: Anorexia spiked during the pandemic, as adolescents felt the impact of COVID restrictions
Family-based therapy for anorexia nervosa supports treatment of the young person in their community, rather than relying solely on hospital admission.
Outcomes for young people tend to improve when their parent(s) are supported to better understand and manage the symptoms of the eating disorder.
It’s about consistency and support
Families are sometimes anxious about joining therapy, often due to fears regarding perceived blame. In reality, clinicians understand most families are doing the best they can with the resources they have.
By integrating parents and other family members in therapy, it is hoped young people will have consistent support between the therapy space and their home environment. Family members can also be important advocates and cheerleaders for their children, as well as challenging symptoms of concern.
Children’s lives and obligations are much broader than ever before. They typically spend a significant time outside of their family and school such as sporting groups, church, social activities and the online space. To provide truly targeted, child-centred care, services will need to consider all domains of the young persons’ world.
Jade Sheen, associate professor, School of Psychology, Deakin University
Amanda Dudley, psychologist and lecturer, Deakin University
This article is republished from The Conversation under a Creative Commons license. Read the original article.


