Why is applying for compensation for psychological injury caused by work at such an emotionally demanding process?
People who have sustained a psychological injury at work face such a Kafka-esque whirlpool of paperwork and pushback from insurers that doctors are advising some patients to stop the claims process and just pay privately for treatment.
“I’ve heard that some GPs are actually reluctant to put people on a WorkCover program because they know what’s coming, which is a shame,” says Dr Terry Lim, a consultant psychiatrist in private practice at The Hills Clinic in Kellyville, NSW.
Dr Lim sees many patients who have been psychologically injured at work and have made successful workers’ compensation claims. For about half of these patients, the nature of their work – as police officers, soldiers, train drivers or paramedics – can expose them to psychological trauma.
“But there is a proportion of workplace injury that has nothing to do with the job,” says Dr Lim.
“It’s to do with bullying from superiors or people you work with. I get librarians from schools and universities with workplace bullying. It can really happen in all industries and all walks of life and all levels. Not-for-profit organisations, they are some of the worst. The disability sector is notorious for very poor workplace processes.”
The primary purpose of WorkCover is to help people get better after a workplace injury and return them to work.
Successful claimants get access to replacement income during their time off work, funding for psychologist and psychiatrist appointments and a case manager to oversee their re-integration into the workforce.
But this support often comes at a cost. The WorkCover process itself can be so traumatic and disempowering that it poses a real danger to the patient’s wellbeing.
“Often, I will give patients the advice to maybe think about stopping the WorkCover process and basically paying for their own treatment with private health insurance,” says Dr Lim.
“Some people can’t do that because of financial reasons. But if they do have the means, at some point I might give them the advice to just get rid of WorkCover if it’s adding too much distress.
“Often, I do see insurers or workplaces that do the right thing in supporting workers appropriately, and that I do see patients returning to work when this happens. But yes, there are problems with the current system.”
DEATH BY PROCESS
Why is applying for worker’s compensation such an emotionally demanding process?
Firstly, there’s the wait.
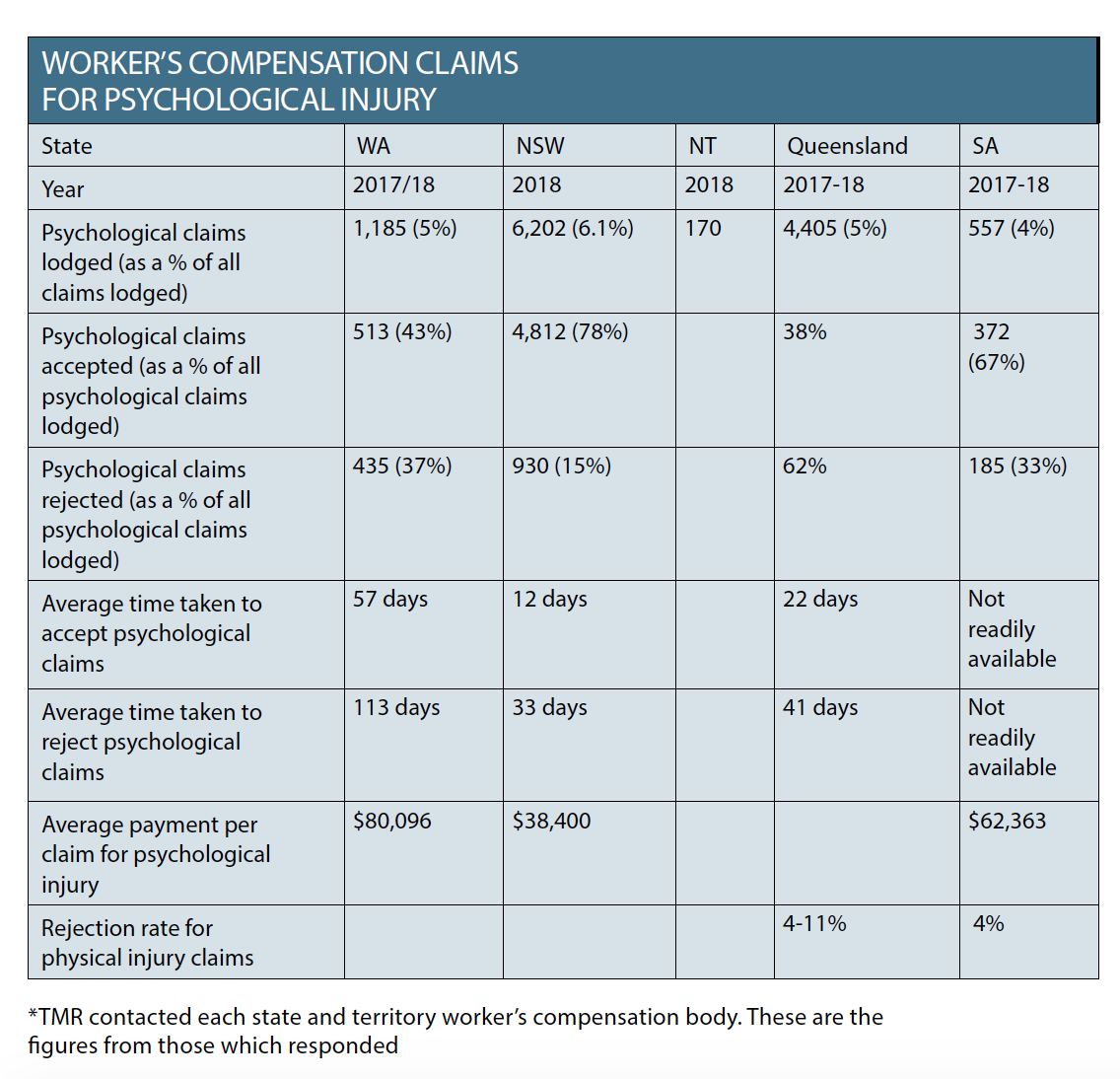
In Western Australia, workers face delays of up to 57 days to have their psychological injury claim accepted and 113 days to have their claim rejected. It’s faster in New South Wales, but Queensland has delays of up to 41 days.
Secondly, there’s the inquisition.
Insurers depend on detailed GP records to make decisions, but they usually still insist on the patient being seen by an independent medical examiner.
Patients are often required to re-live trauma in front of the independent examiner who is paid by the insurer to interrogate them about their illness without providing any treatment.
While some examiners are appropriately sensitive and don’t give patients a hard time, “I’ve heard pretty shocking stories of some examiners whose style is very pugilistic or adversarial,” says Dr Lim.
If the examiner does not believe the patient’s story, that can really upset the patient – who then ends up back at the GP potentially even more traumatised than before, without WorkCover to pay for treatment.
Thirdly, insurers don’t always have the patient’s best interests at heart.
“The whole process of the insurance industry getting involved with a health issue is problematic,” says Dr Lim.
“Obviously, one is driven by profit and budgets and whatnot and that is often at odds with the goal of the treating doctor, which is to get people well.
“There are rehab providers who are being paid by the insurance companies to get people back to work and so it’s obviously governed by things like KPIs around that, which again, may not be consistent with where the patient is at.”
Case managers also change on a regular basis, which disrupts care and creates communication problems between employers, insurers, workers, lawyers, psychologists and GPs.
“Often the barrier for people getting well is not even their clinical condition, it’s having to deal with the insurance company,” says Dr Lim.
Patients do better when they feel they have some level of control over their life and recovery, but WorkCover often removes that sense of agency and responsibility because everything has to be run past the insurer.
Lastly, there’s a reasonable chance that after going through all the pain of getting a compensation claim processed, the claim won’t even be accepted.
Based on data provided by WorkCover Queensland, 62% of psychological injury claims were rejected in 2017-18, compared with 4 to 11% of physical injury claims.
Again, this rate varies greatly according to state, with a claim rejection rate of only 15% in New South Wales and 37% in Western Australia.
NT WorkSafe (the only state or territory regulatory body to accept The Medical Republic’s request for a phone interview) acknowledged that there were significant problems with the process.
“One of the doctors up here calls it ‘compensitis’,” says Kerry Barnaart, the acting director of the Workers Rehabilitation and Compensation Team at the Northern Territory Government’s Department of the Attorney-General and Justice.
“And he said that if you’re not psychologically injured when you go into the system, there is a possibility at the other end that you will be. So that’s a huge concern for us.”
The worker’s compensation process can be time-consuming and “a little onerous” for the GP too, particularly if the independent examiner has a different medical opinion to the GP and the GP is then required to write a dissenting opinion, says Ms Barnaart.
“If a doctor has previously had what they perceive as a bad experience with a claims manager it can make them quite reluctant to be cooperative in the whole process,” she says. “But if they are not cooperative, that actually puts extra pressure on their patient.”
EIGHT DIFFERENT SYSTEMS
To make matters more complicated, every state and territory in Australia has its own version of worker’s compensation and different weekly benefits and liability timeframes.
In the Northern Territory, Western Australia, Tasmania and Australian Capital Territory, the worker’s compensation scheme is privately underwritten, which means that the insurer makes decisions about the claims.
In New South Wales, Victoria and South Australia the insurers work in partnership with government. In Queensland, the worker’s compensation scheme is entirely run by the state.
There’s also a national WorkCover body, Comcare, which covers around 400,000 workers, including all Australian government staff and some employees of private companies.
IS WORK TO BLAME?
When a worker’s foot is crushed on the job, it’s fairly easy for a GP to make a call about whether the injury is consistent with the patient’s story of how it happened, says Professor Louise Stone, a GP based in Canberra who treats WorkCover patients.
Cause and effect may be similarly obvious in the case of an employee who experienced a significant traumatic event at work and now has PTSD, she says.
The same cannot be said for an employee who has been bullied by their boss for years but who also has a pre-existing anxiety disorder and has just gone through a divorce or bereavement.
Mental health problems can creep up gradually and are sometimes the result of compounding, interweaving stresses from work and home life. Sometimes there is no clear cause.
It’s clinically important to make a diagnosis and separate out the possible contributing factors in order to treat a mental health condition, says Associate Professor Stone.
But the worker’s compensation process calls on GPs to make extremely difficult, and almost impossible, clinical judgments that will be depended upon by insurers to determine liability and make decisions about what sorts of tasks a worker is capable of doing, she says.
“If I take seven people with depression, they may have absolutely nothing in common. How do you measure that you have 60% of your concentration compared to your 100% concentration you had beforehand?
“It’s a nonsense in a lot of ways to try and measure mental health in that way.
“And interestingly, here’s a bit of history for you, that’s how the Diagnostic and Statistical Manual of Mental Disorders (DSM) arose. DSM 1 was developed so that the military could quantify how much support soldiers needed when they came back from the Second World War.”
BEING SPECIFIC
As flawed as the worker’s compensation process is, it is important that GPs provide detailed clinical information that can actually be used by insurers and employers to make practical decisions.
The best resource available for GPs is the Clinical Guidelines for the Diagnosis and Management of Work-related Mental Health Conditions in General Practice, released by Monash University earlier this year and approved by the NHMRC, the RACGP and ACRRM.
The guidelines, which were funded (but not influenced) by worker’s compensation bodies in three states and Comcare, contain the most up-to-date diagnosis tools for anxiety, depression, PTSD, alcohol use disorder and substance use disorders.
Making a detailed, formal diagnosis is important as “work stress” is not a condition that can be used in processing a worker’s compensation claim.
“The more background information and specific detail a GP can provide, the better,” says Steve Giddings, the head of workers’ insurance claims at Suncorp, which is one insurance company underwriting worker’s compensation in both territories, Tasmania and Western Australia.
“The GPs report should include all relevant general information such as previous history of mental health conditions, current diagnosis, injury details (if applicable – i.e. secondary or developing mental health), date of first attendance, date of the incident.
“They should also give some consideration for liability – why they believe it to be an injury sustained in the workplace.”
Determining the work-relatedness of a mental health problem is “a notable challenge” for GPs, the clinical guidelines concede.
The best way to tease out the variables was to employ basic logic, the experts interviewed for this story said.
If the worker was succeeding in their career and their mental health went downhill after a change in manager or a particular work incident, it’s hard to argue that the worker just wasn’t capable of dealing with the inherent stress of the job, even if they do have a history of mental health issues.
BACK TO WORK
Psychological injury makes up 7% of all worker’s compensation claims in Australia, and has increased only about 5% in the past 16 years.
But employees with psychological injuries take three times longer than employees with physical injuries to return to work (an average of 17 weeks instead of five weeks, according to Safe Work Australia).
While a swift re-integration into the workforce might be appropriate in some cases, at other times, doctors have to push back to protect the patient.
If the alleged perpetrator of bullying is still employed at a company, for example, a worker may never be able to safely return to that particular workplace.
“There is often little you can do in that situation,” says Dr Lim. “You might work on psychological techniques to build resilience or to manage anxiety better, but it often results in more medication.
“Often, the only way to deal with a toxic work environment is to leave, if they can.”
The consultation room is often where the interests of the insurance company and the interests of the patient come into direct conflict, says Noor Blumer, the national president of the Australia Lawyers Alliance and a personal injury lawyer.
“What is happening a lot – and a lot of doctors will be familiar with this – is that the insurance companies are insisting on sending rehabilitation officers, sometimes even claims officers, along to the medical appointments,” she says.
“Now, that’s a very intrusive thing. And patients don’t understand that they can say, ‘Oh no, I need to see my doctor on my own.’
“Often, the rehab officer will try to argue with the doctor and try to get them to change the certificate to make the conditions under which the person can return to work less strict because that will save the insurance company money.
“Many doctors hate being put in that situation. So, you can understand why doctors are saying to people, ‘I don’t want anything to do with workers’ compensation’.”
It’s actually very rare for a GP to issue a medical certificate that says a patient must not go to work under any circumstances, says Associate Professor Stone. This is usually restricted to notifiable infectious diseases or major trauma.
“But definitely in that scenario where people are saying, ‘I’m starting to have black thoughts’ or the patient who tells you, ‘I was on the top floor of the hospital and I just kept thinking about how easy it would be to just fall off the balcony and it would all be over’, they must not go to work.
“In that circumstance, WorkCover or no WorkCover, they must be off work until they’ve received the treatment that they need.”
There is very little regulation that forces companies to create psychologically safe working environments in Australia.
HARMING FUTURE PROSPECTS
“Unfortunately, while there seems to be more capacity to prosecute companies for not providing safety harnesses or safety barriers, there doesn’t seem to be as many ways of ensuring companies provide the same level of psychological safety in their work environments,” says Dr Lim.
“That probably needs to happen at a legislative level rather than an individual company level.”
Some larger organisations have recognised this problem and are retraining their managers to recognise work practices that are psychologically dangerous.
The Black Dog Institute, for example, is working with industry partners such as Fire and Rescue NSW and state ambulance services to build managerial capability in mental health.
Employees who have been bullied or harassed at work often fear that making a worker’s compensation claim may dash their future employment prospects.
“Patients will say to me, ‘I don’t want to claim WorkCover because I don’t want to prejudice a reference. I’ll just get out of there and not make waves’,” says Associate Professor Stone.
Accessing worker’s compensation often comes at the price of a patient’s privacy, a price which is too high when disclosure could be career-threatening.
For patients with severe psychological injuries who need to take long periods of time off work, worker’s compensation may be the only way to get the support they need.
But for patients who just need some financial help getting through a rough patch, there might be another way.
JobAccess, the national body for disability employment, can provide funding of up to $1,500 per year to employees with specific mental health conditions to access a psychologist for one-on-one specialist support at work.
JobAccess confirmed that employees had successfully accessed this funding in the past 12 months but couldn’t provide specific numbers.
Employees aren’t eligible for JobAccess if they’ve already applied for (or intend to apply for) worker’s compensation.
But, for WorkCover-hesitant patients (who aren’t sure whether their mental health condition is related to work or where work was only partly responsible), it might be worth contacting JobAccess to check their eligibility for support services.