Australia is currently in the midst of a major outbreak of silicosis primarily due to the installation of artificial stone benchtops. This is particularly affecting young and vulnerable workers.
There has been a worrying increase in silicosis cases in Australia recently due to workers being exposed to high concentrations of silica dust from artificial or engineered stone.
The outbreak has been fuelled by the housing boom, and the availability of imported artificial or engineered stone, which is cheaper than natural marble and which comes in many different varieties.
Artificial stone silicosis is a progressive disease characterised by a shorter latency and more rapid loss of lung function than the usual chronic silicosis.1
This disease is entirely preventable through safe workplace practices. Strategies to reduce high intensity silica dust exposure such as dust control, strict enforcement of occupational health and safety regulations and respiratory surveillance of workers are urgently required to prevent further cases from occurring.
BACKGROUND
Silicosis is one of the earliest recognised occupational lung diseases.
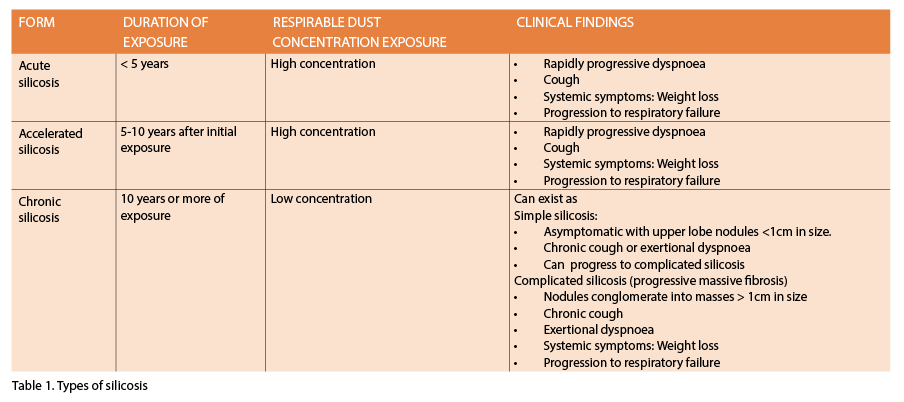
Classical silicosis is a chronic pneumoconiosis (or lung fibrosis due to dust inhalation) which was recognised in the time of Pliny. Four different types of silicosis are recognised. (See table 1 below).
Until recently, cases have usually been older men in industries such as mining, tunnelling, tiling, refractory brick work and the pottery industry. Classically, slowly progressive disease occurs.2
However, recent outbreaks in modern industries, such as sandblasting in denim jean production,3 jewellery polishing4-6 and artificial stone benchtop production and finishing have been associated with an acute accelerated variant of silicosis which is affecting younger workers early in their careers.
Artificial stone (also known as engineered, reconstituted and manufactured stone) is a popular and new building material used primarily in the fabrication of kitchen and bathroom benchtops. The artificial stone is a composite material made of finely crushed elements including quartz as the major filler, with the addition of coloured glass and metals bound together by a polymer resin.7 The silica content of artificial stone is approximately 90%, far higher than natural stones (natural marble 3%, granite 30%).8
Due to its high silica content, very high respirable free silica is produced by mechanical cutting methods, especially if dry cut. Artificial stone has therefore become a source of hazardous silica exposure for workers employed in manufacturing, finishing and installing of artificial stone benchtops.
Since artificial stone first became commercially available, cases of artificial stone silicosis have been reported in Spain,9 Italy, 10 Israel11 and the United States.12
In Australia, the index case was described in 2015, followed more recently by several cases reported in 2017 1, 13, 14; the true prevalence of silicosis is likely to be much higher than that reported in the literature to date. A recent Queensland audit published in February 2019 reported a further 98 cases of silicosis in a four month period, with 15 cases documented to be advanced end stage disease.15
To date, 151 Queensland workers have been diagnosed with silicosis, 25 of whom have progressive massive fibrosis.16 However, there is currently no centralised system for recording disease burden across Australia. Affected individuals in many of the sites of outbreaks have been subcontractors in the building and construction industry or else from a non-English speaking background; these workers seem to have little or no education about risks of crystalline silica dust and have usually been doing dry cutting.
HISTORY, RISKS AND PATHOGENESIS
Artificial stone silicosis is characterised by a shorter latency period and more rapid loss of lung function than chronic silicosis, with the median duration of exposure to artificial stone associated dust being 7.3 years (range 4-10) in one recent Australian study.1
This form of silicosis develops after a short duration but high intensity exposures, and is termed accelerated (or progressive) silicosis. Accelerated silicosis has been comparatively poorly described compared with classical silicosis, but seems to be the type occurring in Australia currently in artificial stone workers.17
While the minimum total lung burden of respirable crystalline silica needed to trigger silicosis is not fully established, the cumulative dose of silica is very important.18 Crystalline silica in artificial stone becomes respirable when disturbed by cutting and grinding.
Much research into the exposure-response relationship between mechanical cutting methods and silicosis has been conducted, but relatively little into artificial stone silicosis. The risk appears greatest when dry cutting is performed19 and at high concentrations (>2mg/m3), even if exposure is brief.20
Once respirable crystalline silica particles are inhaled, they are phagocytosed by alveolar macrophages, causing oxidative stress, apoptosis and upregulation of pro-inflammatory and pro-fibrotic pathways.
This damages the pulmonary parenchyma, leading to the development of fibrosis and permanent distortion of the lung parenchyma, resulting in reduction in gas exchange and eventual chronic respiratory failure.21
Reducing exposure at an early stage slows but may not arrest the natural progression of disease.22
SIGNS AND SYMPTOMS
In the early stages of silicosis, workers are usually asymptomatic. As the disease progresses, however, dyspnoea, dry cough and constitutional symptoms such as fatigue and weight loss may occur. It should be noted that symptoms are often a late manifestation, and many patients are asymptomatic until severe disease is established.
Silica exposure may lead to impaired immune function and increase the risk of other disorders, including tuberculosis, chronic obstructive pulmonary disease, lung cancer, scleroderma, rheumatoid arthritis and chronic renal disease.18 The diagnosis of tuberculosis should be considered in any patient who has come from, or who visits, a country with a high incidence of tuberculosis.
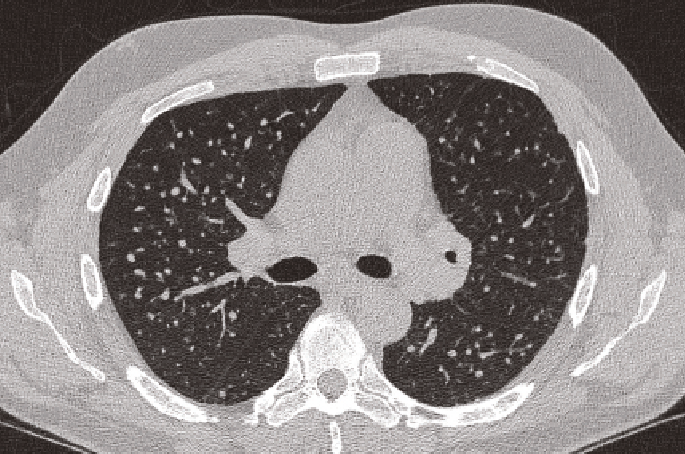
FIGURE 1: CXR and CT scan from the same individual stoneworker with ILO category 3 artificial stone silicosis, illustrating the increased sensitivity and improved diagnostic accuracy of high resolution CT scanning in artificial stone silicosis compared with plain chest radiography. (Reproduced with the kind permission of the patient)
DIAGNOSIS
Diagnosis of artificial stone silicosis relies on a thorough history of exposure to silica dust and compatible radiological features, together with exclusion of other causes.18
Occupational history
A careful and complete occupational history is arguably the most important factor in making a diagnosis. This includes a complete chronological employment and exposure history including a careful account of all jobs worked, with details of the actual tasks performed and dust exposure details. A thorough respiratory and medical history is also essential to assist in excluding other causes. Potential environmental or domestic exposures should also be documented, as well as drug exposures and of course smoking history (and vaping).
Radiology
Chest X-rays have historically been used as the primary imaging modality to detect lung disease due to silica exposure. However, preliminary data from Australian centres caring for workers with engineered stone-related lung disease have found that chest X-rays are failing to reliably detect disease.
One recent study from Queensland found that 43% of workers with International Labour Organisation classified normal chest X-rays had disease visible on computed tomography.23 For this reason, a high resolution CT of the chest is now recommended by the Australian and New Zealand College of Radiologists as the primary imaging modality to be used for screening exposed workers, but has to be performed according to the appropriate technique.24
Computed tomography has higher sensitivity for detecting early disease and greater accuracy in characterising the patterns of disease (See figure 1, above). The interstitial lung abnormalities identified on CT in engineered stone workers are heterogeneous. They can include subtle findings such as small ground glass attenuation and nodules to areas of bilateral progressive massive fibrosis.
Other characteristic findings include centri-lobular nodules, nodal enlargement with or without calcification and pleural thickening.25 A multidisciplinary approach to establishing a diagnosis of interstitial lung disease due to occupational exposure is strongly recommended.24
Respiratory function testing
In the early stages of the disease, spirometry may be normal, and respiratory function testing may not be sensitive enough to detect early lung injury among exposed populations.7, 26. As silicosis progresses, obstruction, restriction or mixed ventilatory deficits may develop.27 The rate of decline in lung function in those with artificial stone silicosis far exceeds the expected rate of decline in healthy patients.28
Serial lung function testing is potentially a way of monitoring progress and predicting prognosis, but has yet to be fully evaluated.
Bronchoscopy and bronchoalveolar lavage
An increased number of lymphocytes and neutrophils characterises the inflammatory process associated with progression in classical silicosis.29 Silica particles and activated macrophages can be also be detected.
Bronchoalveolar lavage in artificial stone silicosis also demonstrates lymphocytosis, with one study finding a cell differential lymphocyte percentage ranging from 31-54% .1 However, such lavage lymphocytosis also occurs in other interstitial lung diseases and silica assessment on bronchoalveolar lavage or histopathology is not always available. No information on the prognostic value of such investigations is available yet in artificial stone silicosis.
Lung biopsy
Thoracic lymph node biopsy can be performed using endoscopic bronchial ultrasound, but again this can be non-specific. Thoracoscopic or open lung biopsy can be used in cases where the diagnosis is uncertain, and is currently the gold standard for diagnosis.
Histology from explanted lungs in patients with artificial stone silicosis has been shown to include the presence of both chronic fibrotic/nodular silicosis and alveolar proteinosis suggestive of silicoproteinosis within the same lung.17
TREATMENT
There is no established effective treatment for silicosis other than supportive care. In recent years, however, lung transplantation has emerged as a potential intervention for end-stage disease.
Several other emerging treatment options are currently being explored including treatment with anti-fibrotic agents.
PREVENTION
Given the absence of specific and curative interventions, it is essential that prevention of unnecessary exposure to respirable crystalline silica occurs. Every effort should be made to reduce dust exposure levels for workers working with artificial stone, and all workplaces with significant exposures are required to undertake independent assessments of personal workplace respirable crystalline silica levels.
The current Time Weighted Average Workplace Exposure Standard (TWA-WES) in Australia and New Zealand is 0.1mg/m3 of respirable crystalline silica over eight hours; however, this was derived from chronic silicosis literature.22
The Australian Institution of Occupational Hygiene, Faculty of Occupational and Environmental Medicine (AFOEM) of the Royal Australasian College of Physicians (RACP) and the Thoracic Society of Australia and New Zealand (TSANZ) have recommended that the TWA-WES be urgently reduced, even as low as 0.05mg/m3.21
At an industry level, all workplaces are responsible for undertaking independent assessments of personal workplace respirable crystalline silica dust levels and implementing measures using the hierarchy of hazard controls to minimise exposure if CFA (coal fly ash) levels are potentially over the limit.30
Three of these measures, in order of effectiveness include: the substitution of hazardous practices to those that are less hazardous (such as sourcing composite stone benches with a lower percentage of silica); the use of engineering controls (wet cutting and local exhaust ventilation); and personal protective equipment with fit testing.
Equipment should meet industry expectations and include work clothing that does not collect dust, and respiratory protective equipment appropriate to the measured silica level.
Generally, a minimum of a P2 efficiency half-face respirator is required to protect against respirable crystalline silica30 and disposable paper dust masks are not effective. 22 Concerningly, occupational practices reported by subjects are not in keeping with those advised by regulatory bodies, with 68% of subjects in a recent Australian study reporting a failure to abide by any hazard controls.23
Government and Statutory bodies also have an important role.
In September 2018, the Queensland government announced a ban on dry cutting of artificial stone and the launch of a health screening program for workers31 as well as a mandatory notification of cases to their central registry. 33
Queensland has also been pro-active in auditing workplaces in the manufactured stone industry, with more than 140 workplaces involved and close to 600 notices issued. 32 Unfortunately, other states have not been as vigilant and there remains no national registry for reporting disease burden. However, the federal government has recently established a National Dust Diseases Taskforce and a central registry is likely to be one of several outcomes.
The Lung Foundation and TSANZ have recently filed a joint submission recommending that similar programs to Queensland (where active case finding is undertaken) should be implemented in NSW and throughout Australia, targeting workplaces involved in manufacturing stone. Victoria and South Australia have recently implemented such programs.
A system is needed for mandatory country-wide notification of artificial stone silicosis which is shared with the regulator, requiring an audit of the workplace of the diagnosed worker and with free respiratory surveillance for the worker.32
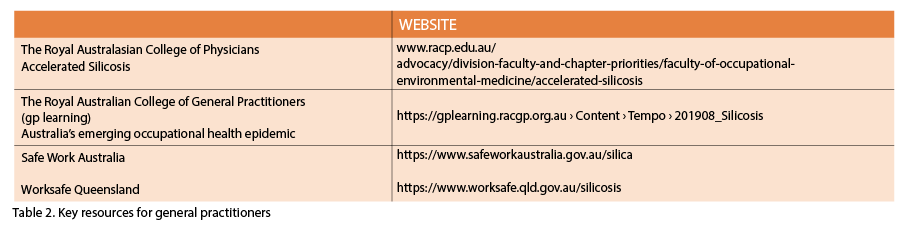
In the interim, the onus falls on medical practitioners to opportunistically evaluate patients by taking occupational histories and enabling early chest imaging. (See table 2 above)
The RACP recommends a full occupational history should be taken from all building industry workers in conjunction with lung function testing (including DLCO) and a chest X-ray.22
Suspected patients should then be referred to a respiratory physician and/or occupational and environmental physician who will then be able to address all the relevant issues including workplace assessment, and potential removal from further dust exposure.
CONCLUSION
Australia is currently in the midst of a major outbreak of silicosis primarily due to the installation of artificial stone benchtops. This is particularly affecting young and vulnerable workers and should not be occurring in the 21st century.
Urgent identification of those exposed to hazardous levels of silica and appropriate health assessments, long term health surveillance programs and personalised management are needed.
Samantha Ennis is a respiratory registrar in the Department of Thoracic Medicine, St Vincent’s Hospital, Sydney.
Deborah Yates is a respiratory physician with qualifications also in Occupational Medicine and Conjoint Associate Professor at The University of NSW.
References
- Hoy RF, Baird T, Hammerschlag G, et al. Artificial stone-associated silicosis: a rapidly emerging occupational lung disease. Occup Environ Med 2018;75:3-5
- Yates D et al: Artificial stone worker’ silicosis: Australia’s new epidemic MJA InSight 2018;
- Akgun M, Araz O, Akkurt I, et al. An epidemic of silicosis among former denim sandblasters. Eur Resp J 2008;32:1295-1303
- Jiang CQ, Xiao LW, Lam TH,et al. Accelerated silicosis in workers exposed to agate dust in Guangzhou, China*. Am J Ind Med 2001;40:87-91
- Panchadhyayee P, Saha K, Saha I, et al. Rapidly Fatal Silicosis Among Jewellery Workers Attending a District Medical College of West Bengal, India. The Indian Journal of Chest Diseases & Allied Sciences 2015;57:165-171
- Murgia N, Muzi G, Dell’Omo M et al. An old threat in a new setting: High prevalence of silicosis among jewelry workers. Am J Ind Med 2007;50:577-583
- Ophir N, Shai AB, Alkalay Y, et al. Artificial stone dust-induced functional and inflammatory abnormalities in exposed workers monitored quantitatively by biometrics. Eur Resp J Open Res 2016;2:00086-02015
- Leso V, Fontana L, Romano R, et al. Artificial Stone Associated Silicosis: A Systematic Review. Int J Environ Res Public Health 2019;16:568
- Perez-Alonso A, Cordoba-Dona JA, Millares-Lorenzo JL, er al. Outbreak of silicosis in Spanish quartz conglomerate workers. Int J Occup Environ Med 2014;20:26-32
- Bartoli D. BB, di Benedetto F., Farina G.A. et al. Silicosis in employees in the processing of kitchen, bar and shop countertops made from quartz resin composite. Provisional results of the environmental and health survey conducted within the territory of USL 11 of Empoli in Tuscany among employees in the processing of quartz resin composite materials and review of the literature. Ital J Occup Environ Hyg 2012:138–143
- Kramer MR, Blanc PD, Fireman E, et al. Artificial stone silicosis [corrected]: disease resurgence among artificial stone workers. Chest 2012;142:419-424
- Martínez C, Prieto A, García L, et al. Silicosis: a Disease with an Active Present. Archivos de Bronconeumología ((English Edition)) 2010;46:97-100
- Matar E, Frankel A, Blake LKM, et al. Complicated silicosis resulting from occupational exposure to engineered stone products. MJA 2017;206:385-386
- Frankel A BL, Yates D.: Late-Breaking Abstract: complicated silicosis in an Australian worker from cutting engineered stone countertops: an embarrassing first for Australia [Abstract]. Eur Respir J 2015;46(Suppl. 59): PA1144.
- Silicosis death dust audit reveals ‘major epidemic worse than asbestos’ [article online], 2019. Available from abc.net.au. Accessed 17/11/2019
- Silicosis and support or stonemasonry workers and employers: Background to silicosis [article online], 2019. Accessed 17/11/19 2019
- Levin K, McLean C, Hoy R: Artificial stone-associated silicosis: clinical-pathological-radiological correlates of disease. Respirology case reports 2019;7:e00470
- Leung CC, Yu ITS, Chen W. Silicosis. The Lancet 2012;379:2008-2018
- Cooper JH, Johnson DL, Phillips ML. Respirable Silica Dust Suppression During Artificial Stone Countertop Cutting. The Annals of Occupational Hygiene 2014;59:122-126
- Buchanan D MBG, Soutar C A. Quantitative relations between exposure to respirable quartz and risk of silicosis Occup Environ Med 2003;60:159-164
- Barnes H, Goh NSL, Leong TL, Hoy R: Silica-associated lung disease: An old-world exposure in modern industries. Respirology 2019;24:1165-1175
- Accelerated Silicosis [article online], 2018. Available from https://www.racp.edu.au/advocacy/division-faculty-and-chapter-priorities/faculty-of-occupational-environmental-medicine/accelerated-silicosis/faqs. Accessed 21/11/2019
- Newbigin K, Parsons R, Deller D, et al. Stonemasons with silicosis: Preliminary findings and a warning message from Australia. Respirology 2019;24:1220-1221
- Imaging of Occupational Lung Disease. Clinical Radiology. The Royal Australian and New Zealand College of Radiologists Position Statement [article online], 2019. Available from https://www.ranzcr.com.
- Cox CW, Rose CS, Lynch DA: State of the art: Imaging of occupational lung disease. Radiology 2014;270:681-696
- Gamble JF, Hessel PA, Nicolich M: Relationship between silicosis and lung function. Scandinavian journal of work, environment & health 2004;30:5-20
- Leung CC CK, Law WS, et al. Determinants of spirometric abnormalities among silicotic patients in Hong Kong. Occup Med (Lond) 2005;55:490-493
- Hoy R: Artificial stone associated silicosis with rapid lung function decline. Eur Resp J 2017;50:OA484
- Paolucci V, Romeo R, Sisinni AG, et al. Silicosis in Workers Exposed to Artificial Quartz Conglomerates: Does It Differ From Chronic Simple Silicosis? Archivos de Bronconeumología (English Edition) 2015;51:e57-e60
- Crystalline silica and silicosis [article online], 2019. Available from https://www.safeworkaustralia.gov.au. Accessed 24/11/19 2019
- Safety alert issued for engineered stone benchtop workers [article online], 2018. Available from http://statements.qld.gov.au/Statement/2018/9/18/safety-alert-issued-for-engineered-stone-benchtop-workers. Accessed 21/11/2019
- Zealand LFaTSoAaN: 2019 Review of the Dust Diseases Scheme. Letter to the Director, Standing Committee on Law and Justice August 2019
- Safe, fair and productive workplaces and communities [article online], 2019. Available from https://qed.qld.gov.au. Accessed 24/11/19
- Australia’s emerging occupational health epidemic – silicosis [article online], 2019. Available from https://gplearning.racgp.org.au/Content/Tempo/201908_Silicosis.