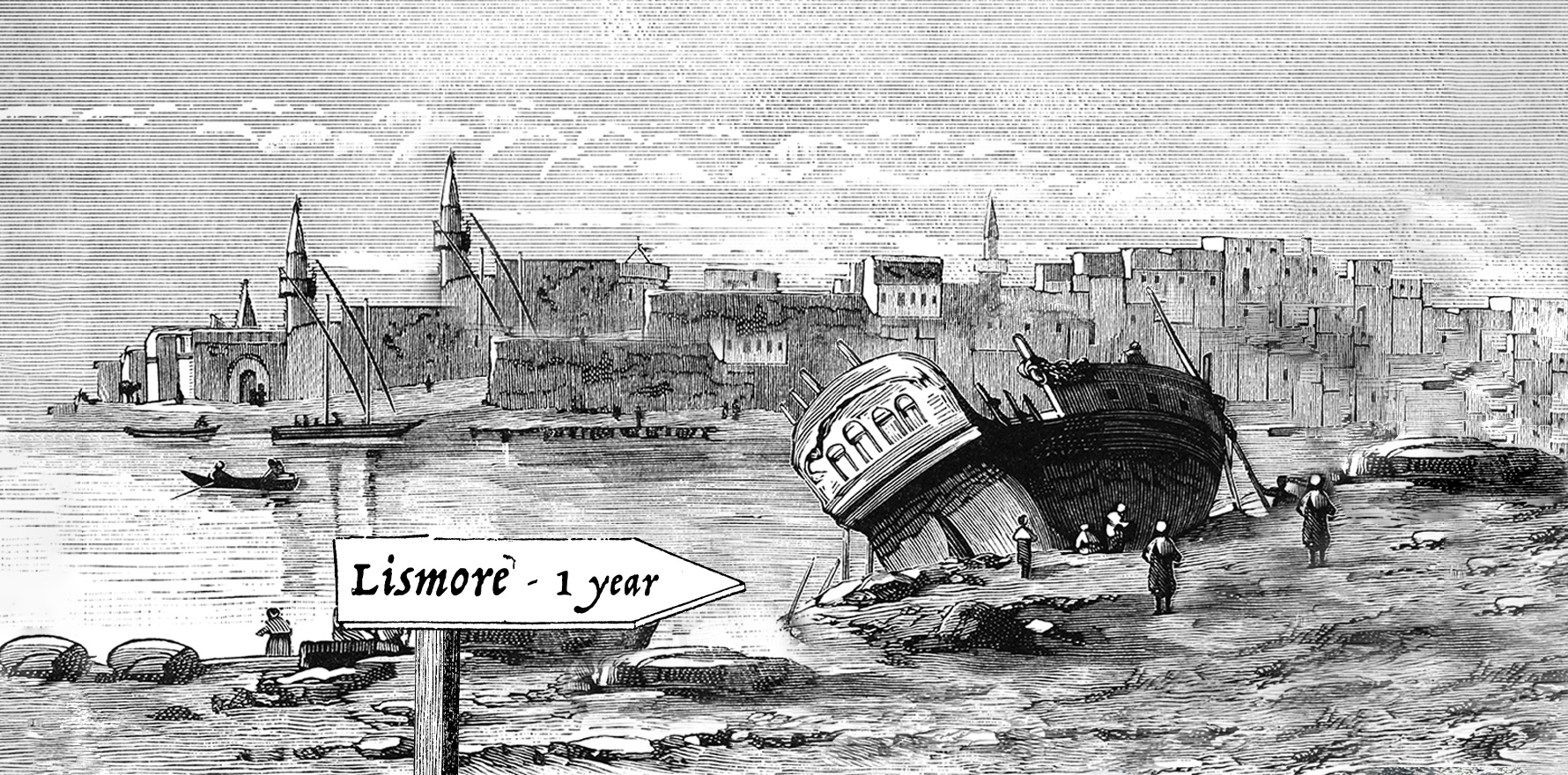
As doctors in northern NSW mark one year since floods wiped out GP practices, patients are presenting with strange symptoms.
Lead poisoning wasn’t something that Ballina-based general surgeon Dr Susan Velovski thought she would see in her career. In the last 12 months, she’s seen at least five cases.
The first patient presented to a local GP with a puzzling set of symptoms, but normal iron levels and an unremarkable colonoscopy.
“I spoke to one of my former bosses about it, who’s like 40 years older than me, and I said ‘it’s like [this patient] has some kind of poisoning’,” Dr Velovski told The Medical Republic.
“And he just goes ‘yeah, lead poisoning’.”
Sure enough, when Dr Velovski’s GP colleague ran more tests, they found basophilic stippling in the man’s blood.
Then it happened again. And again.
Dr Velovski’s patients are based all over the Northern Rivers area of NSW, which was hit by the biggest flood in modern Australian history in late February 2022.
Many are still dealing with the damage.
“People who couldn’t get their insurance to do anything had to find someplace for their kids to stay or to study or whatever, and [now] they’re just scraping out their houses,” Dr Velovski said.
“They’re all Federation houses with lead paint.
“It’s a terrible disease, [lead poisoning].”
Lead poisoning is just the pointier end of the long-term health impact of flooding on the area; poor access to primary healthcare after the flood has created a higher burden of chronic disease.
“When a 60-year-old who previously just had an irregular heartbeat doesn’t get his blood pressure tablets from his GP and ends up with a massive stroke at Lismore Base Hospital, that’s 20 years of good life lost, you’re in a nursing home,” Dr Velovski said.
“They’re the sad things that we’re experiencing as clinicians.”
Another of Dr Velovski’s colleagues, a haematologist, told her that patients were beginning to present with late-stage cancers, thanks to not having been able to see a GP sooner.
Then there are the mental health implications.
“You take a pill for blood pressure, and it will drop your blood pressure and you feel better,” Dr Velovski said.
“But so many cognitive behavioural therapies actually take time and are 30- or 40-minute-long consults with a GP … and they just haven’t been able to set that all up again.”
Only a few acute psychiatric beds are available in the region and the bulk of mental health work is done by doctors in primary care.
“If we could have 20 more psychologists in Lismore – which we can’t – they would be full 24/7 for the next two years,” Dr Velovski said.
Some GP practices, like Keen Street Medical Centre in central Lismore, have only just been able to reopen properly.
“We moved back in on the third of January, having spent the Christmas break moving, physically moving, back,” Keen Street GP Dr Nina Robertson told TMR.
The practice, which went almost completely underwater last year, had to undergo significant works to get back up to scratch.
“Much of the town is still a construction site, so I guess we consider ourselves to be in the lucky number that have managed to get this far in the time that we’ve had,” Dr Robertson said.
A lot of patients, she said, have spent a year with their ruined house, uncertain whether they can or should rebuild where they were.
“The community in terms of housing is still very much in a state of uncertainty, and you can imagine that translates into mental health issues with anxiety and depression,” said Dr Robertson.
Dr Robertson and her colleagues are in a strange place treating these patients, whose depression and anxiety tend to be somewhat justified in the circumstances.
“Sticking together as a community – this is evidence based, it’s not just airy-fairy – but having a meaningful connection and having people who can understand what you’re going through is very important as part of depression treatment in particular,” she said.
“You can’t underestimate the power of just being present with people.”
Most of the time though, Dr Robertson’s patients don’t need to mention the flood directly.
“There’s a shorthand in how we speak about these things, and a lot of it doesn’t need to be said out loud,” she said.
“At this point, there’s an acceptance of where we are as a community.”
Moving back into the Keen Street premises, she said, wouldn’t have been possible without support from the wider medical community, and the practice has even been able to take on new registrars.
“I do want to express my gratitude for that [support], because that has kept us going in the absence of support from elsewhere,” Dr Robertson said.
While there was an initial injection of cash in the immediate aftermath of the natural disaster, both Dr Robertson and Dr Velovski said that recovery funding seems to have dried up.
So far, GPs and other health services have only been able to access a nonspecific grant for flood affected business owners.
Late last year, NSW Rural Health Minister Bronnie Taylor wrote to the federal health minister on behalf of the NSW Rural Doctors Network, advocating for a primary care-specific grant.
Health Minister Mark Butler confirmed with Ms Taylor in October that the Department of Health would consider a proposal for a new Healthcare Flood Recovery Grant, which would be jointly funded through the Northern Rivers grants program.
Janelle Saffin, the state member for Lismore, has also taken up the cause.
“I continue to advocate on this, as all sectors of our community need support,” she told the Lismore App in January.
“The health sector in particular need it so as they can best support our community’s health and medical needs. They were smashed along with everyone else, in quite exceptional circumstances.”
Ms Saffin said she had received “positive signals” from Mr Butler immediately before Christmas, but nothing has been announced so far.
Dr Robertson fears that the politicians holding the purse strings will never understand what it’s like on the ground in Lismore.
“I don’t really think [many politicians] understand that the healthcare system is one entity,” she said.
“They tend to separate the bits they fund directly from the bits they don’t, and we’re obviously part of the stuff that they don’t fund directly.”
Dr Velovski, meanwhile, has an invitation for the politicians to come and see what a world without good access to general practice actually looks like.
“Come and walk in our shoes,” she said.
“Not for a half an hour or until the next plane out but stay here a week and see how it’s been affected.”