More than a third of migraine sufferers would benefit from prophylactic treatment rather than overly rely on analgesics, writes Dr Bronwyn Jenkins
Migraine is a common and debilitating condition. As a worldwide cause of disability measured in years of life lost to disability (YLD), migraine is ranked second, contributing 40.8 million to 75.9 million total YLDs.
From the Global Burden of Disease 2016 study, migraine was the sixth most prevalent disease, with an estimated prevalence of 1.04 billion.1 Prevalence rates of migraine in Western countries vary from 4% to 9.5% in males and 11.2% to 25% in females.2 The prevalence of chronic migraine ranges from 1% to 3% in studies.3
In a study of migraine management in Australian general practice 10 years ago, there was a prevalence of 11.5% of patients diagnosed with migraine, with 12.3% of these reporting three or more migraines a month, yet only 19.7% of this group were taking prophylactic medication at that time.4 Similar to other international studies, this suggests that migraine remains an under-treated condition, particularly since it is estimated that approximately 38% of migraine sufferers would benefit from prophylactic treatment.5
In contrast, patients were overusing analgesics, including 38% of the Australian patients in this study taking opioid-combination analgesics, many of which have been readily available over the counter in Australia until now. In addition, 9% of the patients reported using their acute analgesics as prophylaxis.4
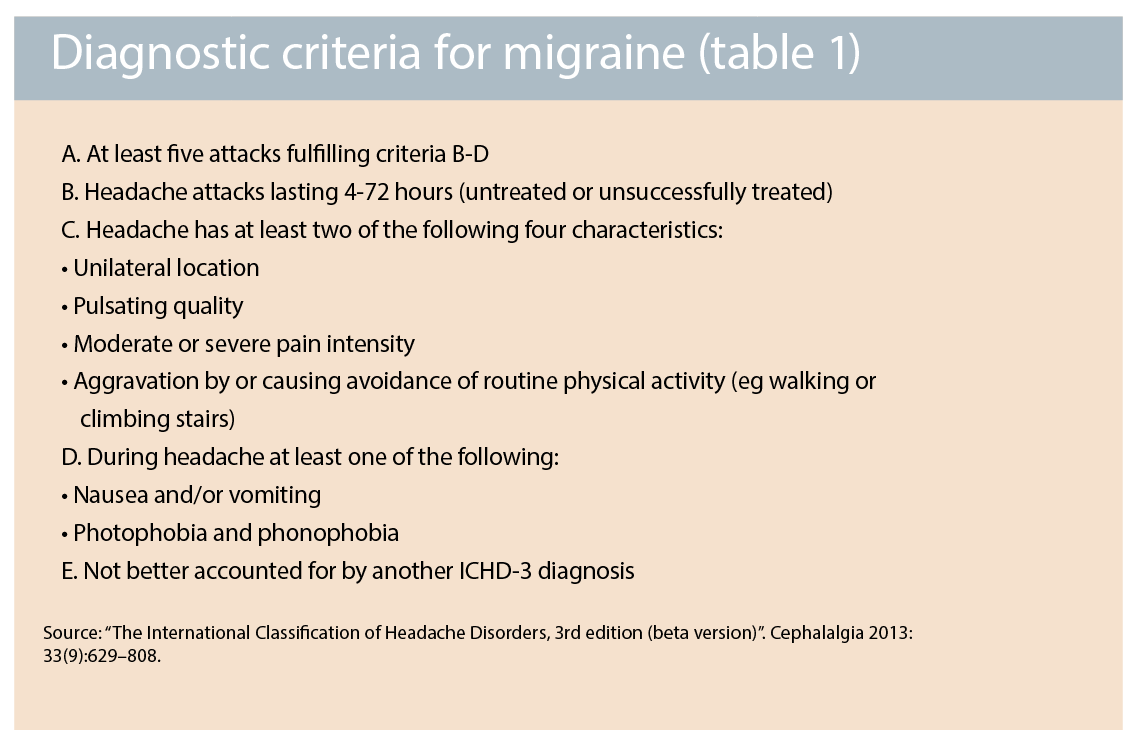
Diagnosing migraine is dependent on clinical features from the history. Migraine is defined as episodic ( less than 15 days a month) or chronic (15 or more days a month), with or without aura. The current definition encompasses a headache often lasting four to 72 hours without treatment, with some features of being unilateral, pulsating or moderate/severe pain and avoidance of activities; as well as nausea or sensitivity to light and noise (photophobia and phonophobia).6
It is of note that the person does not have to have all of these features during all of their headaches to qualify as having a migraine. (See table 1)
There are many effective acute therapies for migraine and these medications generally work better when taken early in the migraine attack. There is evidence for the use of:
• Antiemetics, such as metoclopramide or prochlorperazine; to alleviate the vomiting and facilitate absorption of the other oral medications if nauseated. (level B evidence)
• Paracetamol for milder headaches, particularly in combination with metoclopramide and ibuprofen
• Non-steroidal anti-inflammatory medications such as ibuprofen, acetylsalicylic acid, naproxen and diclofenac (level A evidence).
• Triptans, particularly for moderate or severe attacks, including sumatriptan (available as oral tablets, distintegrating tablets or nasal spray on PBS), rizatriptan (a disintegrating tablet), eletriptan, zolmitriptan and naratriptan (the latter three all being oral tablets). (Level A evidence) 7,8
Prophylactic treatment should be considered for patients with more than three days per month of headache related disability, or for patients who have less frequent but ineffectively treated severe attacks.9
Migraine prophylactic medications are aimed to decrease the frequency and severity of the migraine attacks.
Current prophylactic recommendations include:
• Antiepileptic medications: such as, topiramate (level A evidence); sodium valproate (level A evidence); gabapentin (level B evidence)
• Antihypertensive medications: propranolol (level A evidence), verapamil (level B evidence), candesartan.
• Antidepressant medications: amitrypitiline (level A evidence), nortriptyline (level C evidence)
• Pizotifen
• Natural supplements: magnesium, vitamin B2 and others (level B evidence)
• Onabotulinum toxin A (Botox): authorised in Australia for patients who have chronic migraines, having failed more than three other migraine prophylactic medications, when given by a neurologist (level A evidence).
The choice of prophylactic treatment should be individualised depending on patient choice, tolerability and effectiveness. For example, an antihypertensive would be more ideal for a patient with hypertension; a medication with sedative side effects could be used at night for patients with initial insomnia; an antiepileptic causing decreased appetite rather than weight gain may be more suited to an overweight patient; or contraindications such as asthma would preclude the use of propranolol.
Acupuncture, relaxation training, biofeedback and cognitive behavioural therapy may also be useful (level A evidence). Management of any comorbid factors such as anxiety, depression, insomnia, sleep apnoea, hormonal changes, temporomandibular joint dysfunction or neck issues are also important in some patients.
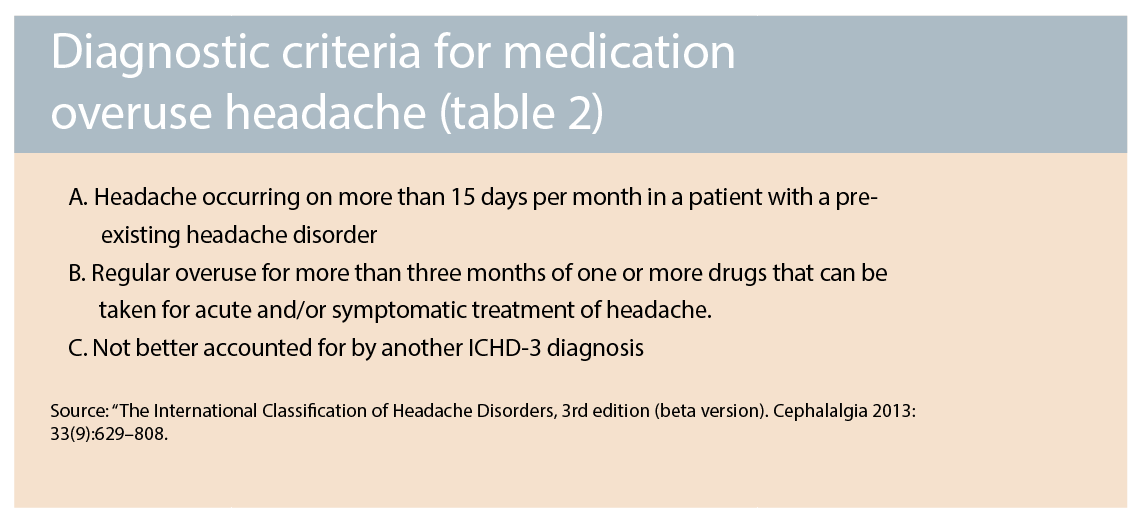
However, about 2.5% of people with episodic migraine transition to chronic migraine each year. Risk factors for developing chronic migraine include: non-modifiable risk factors of older age, female gender, Caucasian ethnicity, low socioeconomic status, genetics; and potentially modifiable risk factors of obesity, snoring, head or neck injury, depression and major stress.9 With increasing headache frequency there is an increased requirement to treat the migraines effectively. In addition, frequent use of analgesics can further increase the vicious cycle, with a secondary diagnosis of medication overuse headache (See table 2).6
In international studies, there is an estimated prevalence of 1% to 2% for medication overuse headache, as high as 7% in some studies.10 Up until now, the availability of codeine over the counter in Australia has enabled patients to increasingly self-medicate, adding to the frequency and severity of their migraines with medication overuse. In general, opiates should not be used for the routine management of migraine, with other medications being potentially more effective for attacks with less potential for medication overuse headache.7
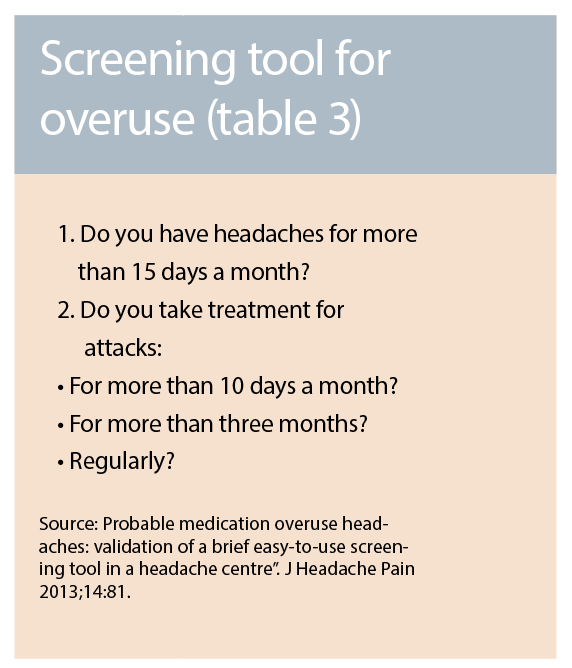
Recognising medication overuse headache is the first step in its management.A simple screening tool was able to correctly identify medication overuse headache in 86% of patients, with a specificity of 79% 11
Currently these patients are often presenting to their pharmacist first, so a multidisciplinary approach including pharmacists to direct them to their doctor for other treatments can be useful.12 First-line treatment of medication overuse headache is management in primary care, with a brief intervention of simple advice and education.
A study of 25,486 patients in Norway showed that a brief intervention by the general practitioner was effective, with resolution of chronic headache in 50% of the group receiving the intervention, compared with 6% in the control group.13
The intervention was information provision about the risk of medication overuse headache, the benefits of treating it, negotiation of diarising headache and analgesics, and a written plan including a contact for support. More complex cases may require specialist care for inpatient or outpatient detoxification, such as: those who have failed outpatient detoxification; prolonged overuse, particularly of opioids; or other comorbidities. In either setting, patient education and support are helpful in limiting pain medication use and preventing relapse.14
In order to avoid medication overuse leading to migraine chronification, we should inform our patients that analgesic use of 10 or more days a month of codeine or triptans can increase headaches. If medication overuse is already established, it is fair to negotiate realistic expectations for initially worsened headaches after detoxification, for usually two to 10 days (average 3.5 days),15 but this may continue for two to four weeks in some cases.
This initial worsening is more than compensated for by expected improvements in the frequency and severity of the headache for many patients after the initial detoxification stage, which can take up to 12 weeks or longer. Positive predictors for successful treatment of medication overuse headache include: migraine as the primary headache; chronic daily headache lasting less than 10 years; and ergotamine as the overused medication.
Significant improvement in headache frequency and intensity after withdrawal of the overused medication varies from 45% to 61%. Ongoing education and support is necessary for these patients since there is a relapse rate of medication overuse within the next five years of 40% to 60%.15
Comparative studies of interventions in medication overuse headache are ongoing, but a recent systematic review of studies on medication overuse headache between 2004 and 2014 suggested that the best treatment is to discontinue the overused medication with the addition of preventive medication.14 This is a common strategy in Australia; while other countries mainly use preventive medications after detoxification, on the basis that some patients may not need headache prophylactics if significantly improved by the withdrawal alone.10
With the requirement for a prescription for codeine after February 1 next year in Australia, patients will increasingly present to their trusted general practitioner for medications.
As doctors, we naturally want to help ease our patients’ suffering so the temptation may be to offer analgesics of progressive potency to alleviate their pain.
The severity of the pain of the migraine should be validated to the patient, rather than minimised. Communicating an understanding of the debility of migraine can aid in negotiating better alternative strategies for the individual. Reducing the severity and frequency of headaches can facilitate the use of simpler analgesics or non-medication strategies instead of narcotic analgesics.
With education, restriction of codeine to a script will be an important opportunity for doctors and patients to provide and access better treatment for their migraines.
RESOURCES FOR PATIENTS
• Information and a register for migraine patients is available at http://headacheaustralia.org.au/migraine
• An easy to use but informative headache diary for patients is available at www.aspenpharma.com.au/patRes/2014_Headache_Diary.pdf
RESOURCES FOR DOCTORS
• TGA resources providing practical suggestions on how to redirect treatment from codeine to other simpler analgesics and other non-medication strategies is available at: https://www.tga.gov.au/tips-talking-about-codeine-guidance-health-professionals-prescribing-authority
• American Headache Consortium Guidelines is available at http://eguideline.guidelinecentral.com/i/76857/5=
• ICHD-3beta with information on headache classification and tips is available for download at: http://www.ihs-classification.org/_downloads/mixed/International-Headache-Classification-III-ICHD-III-2013-Beta.pdf
Dr Bronwyn Jenkins, is a neurologist at the North Shore Vertigo and Neurology Clinic, St Leonard’s, NSW, and co-secretary of the Australia and New Zealand Headache Society
Disclosure: Dr Jenkins has previously received consulting fees from Allergan and Novartis and lecturing fees for Allergan and Boehringer
References:
1. GBD 2016 Disease and Injury Incidence and prevalence Collaborators. “Global, regional and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016”. Lancet, 2017 September 16; 390: 1211-1259.
2. Younger Ds. Epidemiology of Migraine. Neurol Clin, 2016; 34: 849-861.
3. Natoli JL, Manack A, Dean B, et al. “Global prevalence of chronic migraine: A systematic review”. Cephalalgia, 2010; 30: 599-609.
4. Stark RJ, Valenti L, Miller GC. “Management of migraine in Australian general practice”. MJA, 2007 August 6; 187: 142-146.
5. Lipton RB, Bigal ME, Diamond M, et al. “Migraine prevalence, disease burden, and the need for preventive therapy”. Neurology. 2007; 68: 343-349.
6. Headache Classification Committee of the International Headache Society. “The International Classification of Headache Disorders, 3rd edition (beta version)”. Cephalalgia 2013: 33(9):629–808.
7. Becker WJ. “Acute Migraine Treatment”. Continuum, 2015; 21(4):953-972.
8. Silberstein SD for the US Headache Consortium. “Practice Parameter: Evidence-based guidelines for migraine headache (an evidence-based review): Report of the Quality Standards Subcommittee of the American Academy of Neurology”. Neurology, 2000; 55: 754.
9. Lipton RB, Silberstein SD. “Episodic and Chronic Migraine Headache: Breaking down barriers to optimal treatment and prevention”. Headache, 2015; 55; S2:103-122.
10. Westergaard ML, Munksgaard SB, Bendtsen L and Jensen RH. “Medication-overuse headache: a perspective review”. Ther Adv Drug Saf, 2016; Vol 7(4):147-158.
11. Dousset V, Maud M, Legoff M, Radat F, Brochet B, Dartigues JF et al. “Probable medication overuse headaches: validation of a brief easy-to-use screening tool in a headache centre”. J Headache Pain 2013;14:81.
12. Stark RJ, McGuire T, vanDriel ML. “Medication overuse headache in Australia: a call for multidisciplinary efforts at prevention and treatment” Medical Journal of Australia, Sep 19 2016; 205(6):283.
13. Kristoffersen ES et al. “Brief intervention for medication-overuse headache in primary care. The BIMOH study: a double-blind pragmatic cluster randomised parallel controlled trial”. J Neurol Neurosurg &Psych 2015;86(5):505-12.
14. Chiang C, Schwedt T, Wang S and Dodick D. “Treatment of medication overuse headache: a systematic review”. Cephalalgia, 2016; 36:371-386.
15. Dodick D, Silberstein SD. “How clinicians can detect, prevent and treat medication overuse headache.” Cephalalgia, 2008;28: 1209-1217