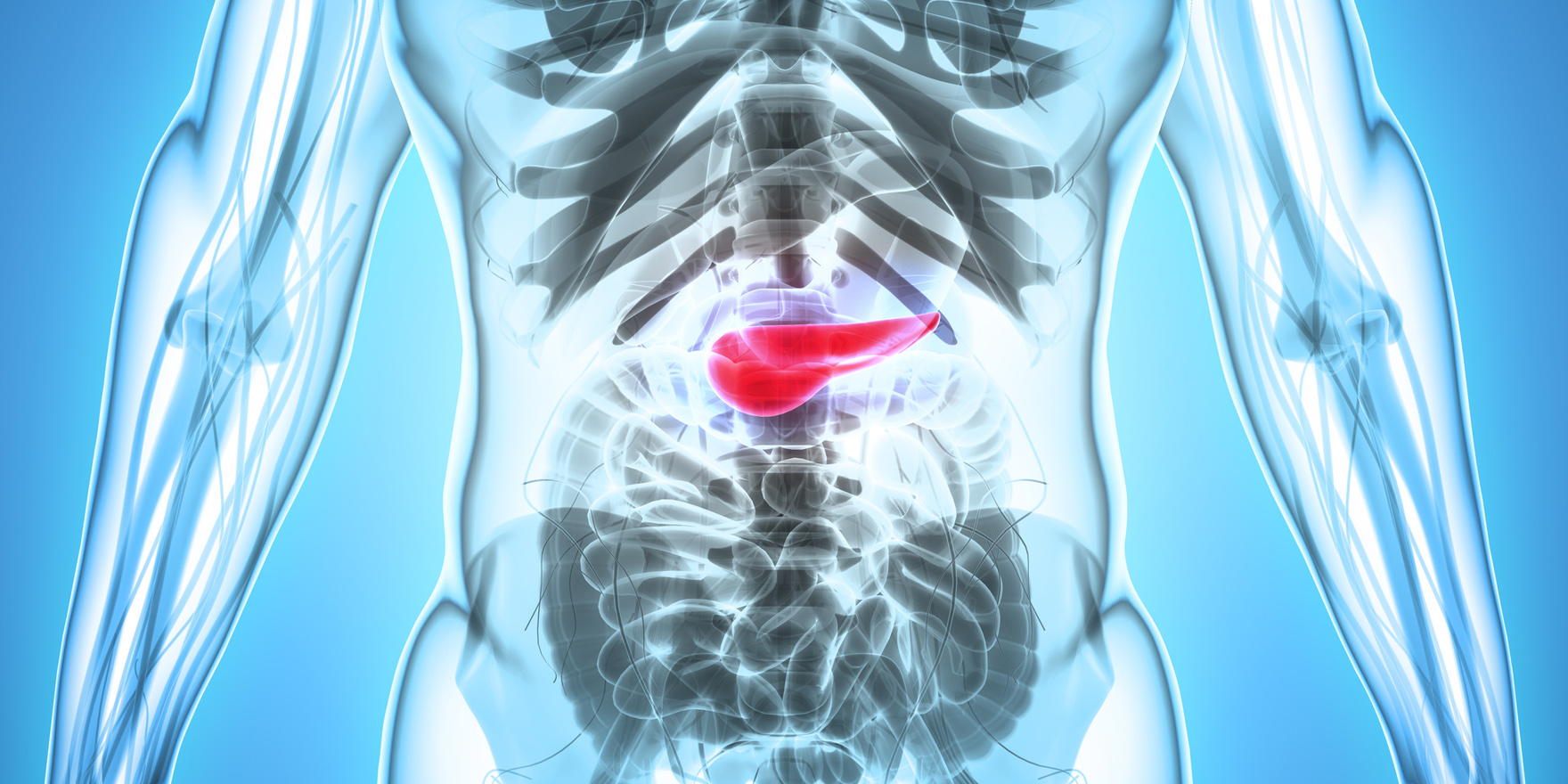
The incidence of diabetes after pancreatic disease is more common in adults than type 1 diabetes, but it may be under-recognised
The incidence of diabetes after pancreatic disease is more common in adults than type 1 diabetes, prompting concerns the former condition may be being under-recognised and mismanaged.
University of Surrey researchers urged clinicians to be alert to the condition, after their analysis of more than two million UK primary-care records revealed only 2.7% of diabetes diagnoses post-pancreatic disease were correctly labelled diabetes of the exocrine pancreas.
“Recognising the role of pancreatic damage in the development of a patient’s diabetes is vital to inform appropriate management plans,” the researchers said. “Most patients were labelled type 2 diabetes, despite a seven-fold increased insulin requirement within five years, by which time 45.8% of patients with diabetes after chronic pancreatic disease are using insulin.”
Without a quick transition to insulin, these patients risked “devastating long-term effects” such as eye, kidney and nerve damage, they said.
Diabetes of the exocrine pancreas, also known as type 3c or secondary pancreatic diabetes, occurs after damage to the pancreas. Changes such as pancreatitis, surgical resection or abnormal growth disrupt the pancreas and affect the exocrine and endocrine functioning.
And while it was nowhere near as common as type 2 in the community, one in 10 hospital patients with diabetes were thought to have it.
Professor Jonathan Shaw, spokesperson for the Australian Diabetes Society and deputy director at the Baker Heart and Diabetes Institute, said the lack of a test differentiating this sub-type from usual type 2 diabetes meant vigilance was important.
“Knowing that a person has a condition which predisposes them to require insulin does influence the doctor-patient interaction,” he said. “It makes you less likely to assume that the reason you’ve got poor control is because the person is non-compliant with their diet and exercise.”
The study revealed a heterogenous group of people with the condition, including those diagnosed in middle age and in the obese category, as well as those who were younger and of normal weight.
While acute pancreatitis was the most common pancreatic disease in those diagnosed, the injury could be from any number of causes, the authors said, adding that evidence suggested the more severe the organ’s injury, the greater the impact on insulin production.
Professor Shaw agreed with the study authors’ concerns that misdiagnosis could lead to safety concerns, given the open question around whether GLP analogues and DPP4 inhibitors led to pancreatitis.
Nevertheless, the study finding that many of the clinicians progressed their patients to insulin quickly indicated that, though they might have been coded in the patient notes incorrectly, many were still being treated appropriately, he said.
“As a clinician I may recognise that it’s almost impossible to tell whether the diabetes which occurred a couple of years after pancreatitis is or isn’t related to that pancreatitis.”
Instead, recognising the patient had pancreatitis in the past can prime the doctor to quickly move them to insulin if they were not getting good control with tablets.
Diabetes Care; online 23 October