Futurists might have doctors’ incomes and status heading for the chopping block, but actually it’s mostly good news
While some categories of doctor face severe disruption with the march of digital technologies over the coming decade, the future of general practice is surprisingly bright
Doctors, lawyers and accountants who are just starting their careers must be a little nervous. They are the poster children of digital disruption doomsayers who reckon these three professins are in a lot of trouble over the coming decade.
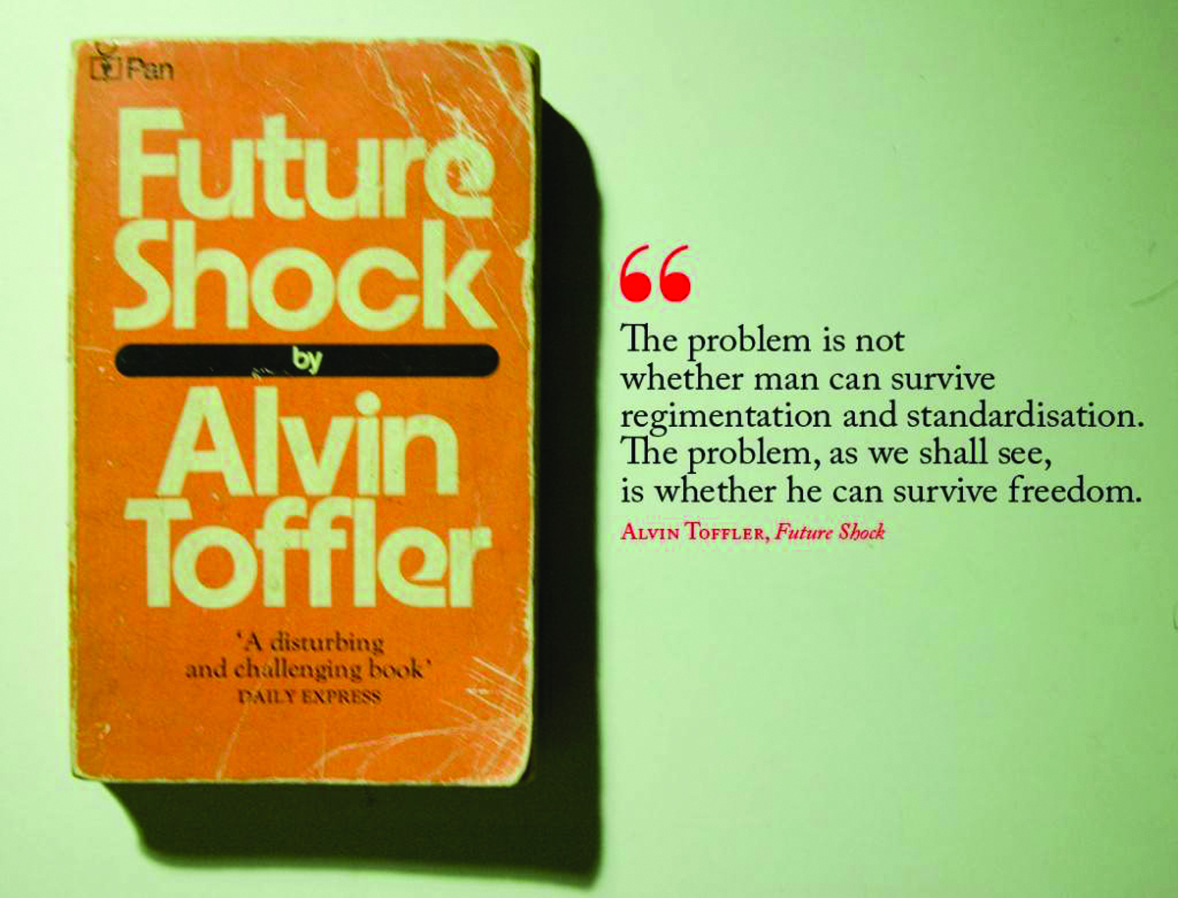
As a survivor, so far, of an ongoing digital media apocalypse, I think I might have an inkling of what a young GP could be thinking reading this. My denial wavered from: “Not going to happen like that, I read Alvin Toffler’s seminal 1970s classic Future Shock, it was all bollocks in the end” to “I love the internet, I’m sure there’s a good spot for me in there” all the way through to “It’s a nightmare, why wasn’t I warned, I need a long holiday in a tropical paradise to help me forget.”
The trouble with writing a piece like this is, if you scare your readers too much at the start, they will stop reading.
After all, it’s just speculation, right? Just like Future Shock.
Here’s some speculation from a couple of Oxford University researchers writing recently in the Harvard Business Review. They say that “within decades the traditional professions will be dismantled, leaving most, but not all, professionals to be replaced by less expert people, new types of experts, and high performing systems”.1
Relax and read on. This is largely, a good news story – for GPs at least. And all of the thinges in our list below are mostly already starting to happen, so there is some logic to believe some of the forecasts.
The bad news is, it’s still a lot of change, and if you don’t plan for it, you might end up in “the land that time forgot”.
Our general prediction: In 10 years’ time, general practice, won’t look at all like it does today. But, on the plus side, it will be a major thriving profession and will likely be a more interesting profession than ever before, and much better paid.
This doesn’t mean you can relax. Big changes are coming, and big change is scary.
You probably need to do a bit deeper thinking and planning around these major potential shifts in your working life, especially about the role innovative technology can play in your future.
The changes listed here are not necessarily in order of impact.
1. Generalism will rise over specialism
Anything that is primarily knowledge-based, particularly “deep and vertical” knowledge-bases (such as specialism in medicine) is a target for automation and machine learning. If you can’t beat Big Blue at chess any more, the once hallowed grounds of specialism are clearly now susceptible, in some sectors, to brute processing power, big data processing, and increasingly elegant self-learning algorithms. We are already seeing a very rapid replacement of imaging-based specialists by machines, for the simple reason the machines now get it right far more consistently and accurately than humans do.
It’s just the beginning though.
Our healthcare funding won’t suffer the current imbalance between specialism and generalism. As healthcare becomes more and more distributed through connected digital technology, the need for savvy multidisciplinary doctors (generalists), will be much greater. Depending on what type of specialist you are, your career will be decidedly trickier to navigate and almost certainly less well paid in relative terms to GPs today.
Technology is the generalists’ friend, even if you think that you, too, are mainly a knowledge-based worker. Technology will get rid of boring tasks, ones which might or might not be taken by machines, but can be performed by pharmacists and nurses at least. That means using technology, the GP will competently, and with enough time, do more of what the specialists do now in their everyday work.
The core of this change is the rising rates of chronic disease and the need for different care and funding models to manage its scale and distribution.
Care is much more efficient at its point of origin, so GPs are perfectly placed to start managing chronic care far more.
Some adjustments just need to be made in how GPs are trained, educated throughout their career and how they are paid.
Hints:
• Don’t be scared of AI and machine learning. It’s not like you’re a radiologist. You’ll need it in your generalist kit bag. It will likely help you process certain categories of patients faster, so you can optimise income and spend more time on more complex patients.
• Chronic care management is going to be a centrepiece of a lot of GP work as it is now. Set yourself up for it. That means digital networking with every profession around you that is relevant in a care team. That means being digitally savvy.
• Don’t be so fussed about pharmacists and nurses taking more manual jobs, such as vaccinations. Did you like doing those anyway? Let them handle that stuff.
2. Telehealth will always be on and paid for
If you’re going to be efficient and make more money, telehealth is probably in your future as a GP. But there’s a change of mindset needed here. Currently many GPs decry most telehealth start-ups as denuding the vital patient-doctor relationship. Some of them probably do this. But there are others, such as GP2U and Welio, which are strictly GP-centric. Eventually, with enough doctors on a telehealth network, Uber-like algorithmic patient processing for certain categories of patient will be possible. In other words, a patient wants something which is a low-risk request, but important to them, such as a repeat of their long-term statin, and theywant rto see a doctor “on demand”. These systems will start by connecting you with your patients, then your patients with your other practice doctors if you aren’t available, then they will move to algorithms to find other “most suitable” GPs (maybe recommended by you, or using combinations of factors like this and geolocation).
The point is, a patient taps their phone and gets a doctor like they get an Uber. This will happen. It’s started already. The bad side is the regulation to ensure continuity of care, as patients should be mostly seeing their regular trusted GP. They are the ones more likely to pick up something funny, even on a phone call.
The good side, is that these systems make all telehealth now a paid service. In a survey recently conducted by The Medical Republic over 80% doctors admitted to doing different forms of telehealth for which they weren’t paid. Imagine if you’re paid for everything you do, even if it’s just a small amount, for a small thing.
Technology is already set up for doctors to do that, as businesses such as Welio and GP2U have demonstrated. And the better news is, the amount of items reimbursed on the MBS for telehealth consults will almost certainly increase because the government would be mad not to do it. It’s game-changing, in terms of efficiency.
Lastly, if you run telehealth well, you will get more patients, who are happier and more willing to pay for upgraded convenience. At the moment after-hours doctors’ services are breeding like rabbits, and a large part of this is convenience.
Hints:
• There is nothing wrong with making things more convenient for you and your patient using technology if you do it properly and set up the appropriate internal governance regime.
• Telehealth is a new source of relatively easy income. You do it already. Get a system and get paid for what you do.
• Telehealth, managed correctly, will increase patient satisfaction and practice income.
3. EQ trumps IQ now
Highly skilled workers such as doctors command high rates of pay because of three things: their learned knowledge; their combination of experience and knowledge in making decisions;, and their communication and relationship skills in helping their patients navigate the right medical journey.
AI and machine learning are going to kill off much of the first two eventually. By that, experts say, not today, but at least within 10 years. That leaves the last one. EQ stands for emotional quotient. It is a measure of relationship, communication and empathy skills.
GPs already have a role that is defined as “having to know everything”. But innovation is happening at such speed, keeping up is practically impossible. Even specialists, with their narrower focus, can’t do this.
To stay in the game, GPs will likely need to embrace machine help a lot more . When they combine this with their existing continuity of patient relationships they will be able to move upstream into even more complex clinical management challenges. They wll essentially begin to inhabit pockets of what traditionally has been specialist territory.
GPs are ideally positioned to make this move because their every day job has always required them to be well versed in the arts of pursuasion, empathy and listening. Their patient relationships are longitudinal not short term and vertical as they are with specialists.
The combination of this and using AI and machine learning to assist them with more complex knowledge based diagnosis will make their effectiveness in the overall healthcare system even greater than it already is.
Hints:
• Learn to use and embrace AI and machines where they are useful to you and learn to know where the line of relationship and understanding takes over.
• Start thinking of your patients in categories of relationship for return on their health and your income.
4. AI and Machine Learning are your friends (usually)
“Any doctor who can be replaced by AI and machine learning, should be replaced by AI and machine learning”, Dr George Margelis told this year’s Australian Telehealth Conference.
That’s not a bad summary if you look under the hood of what he is getting at. In the case of radiologists and some other imaging specialists, unfortunately, they probably will need to be replaced, and pivot their profession to other functions such as interventions, as interpretation of data and results is going automated. But for the vast majority of GPs this statement means that while machine-learning will replace big components of what they do today, they should be embracing this and moving upstream, with the efficiency opportunities and additional time this technology will offer them.
For GPs, AI is much more an opportunity than a threat, if it is embraced properly. GPs who feel threatened by this technology usually resort to the argument that it undermines the universal need for face-to-face doctor sessions in order to ensure accurate diagnosis and continuity of care. That’s all nice, but it can be significantly inefficient, and in a fast-changing world of increasing consumer demand and an escalating chronic disease-ridden ageing population, impractical. There are sicker patients who need more attention, and computers are getting accurate at managing the not-so sick ones.
Hints:
• Think a bit more laterally about AI, machine learning and the cloud. It’s not all Minority Report and Ex Machina.
• Population growth and chronic care loads mean there aren’t enough doctors and never will be, even in Australia. You are needed and will be the hub of efficient care.
• Technologies will make this problem more manageable here and open up medicine to vast populations in the Third World countries.
5. The RACGP won’t exist
Just kidding. That might get the College’s attention though, because how it manages the training of GPs now, and their life-time learning, is stuck somewhere in the Seventies. Of all the changes that might affect GPs in the next 10 years, life-long learning might just be the biggest one they will face. Which is why one would expect the RACGP might be little more leading edge than it is today.
In some ways, the RACGP is a classic incumbent. It is making a lot of money and has traditional structures and power plays in place. There is no immediate requirement to change. The leaders in this organisation aren’t on a “burning platform” like some of the leaders in disrupted business sectors. The problem is disruption of its incumbency has been prevented by its virtual monopoly on the training and education of GPs. This has effectively trapped GP learning in a time bubble and holds back the profession from embracing the efficiencies and advantages of digital transformation.
But we predict that bubble will burst and the RACGP will eventually change. It has to. Already disruption is creeping across its bow. Witness GPs Down Under(GPDU) vs ShareGP. One is a hub of communication activity and learning with massive GP engagement. The other pretty much has tumbleweeds rolling through it. People will work these issues out eventually and change things.
Some trends are clear:
Social media based peer-to-peer learning and CPD (mostly free)
We see it in some organisations in the GP realm, for example, GPDU, a Facebook group started with the major aim of educating GPs and registrars who felt isolated, put upon at times, and restricted by old learning models. Powerful groups such as FOAMed (Free Open Access Medical Education) and SMACC (Social Media And Critical Care) are exploding in other areas of medicine, such as emergency care, and eventually GPs, and their training organisations will need to embrace these models.
Data guidance of learning needs and personal development, particularly self reflection
Automated data collection will do more than freeing doctors from having to manually input and manipulate data on their current desktop patient management systems. Currently, the NHS in the UK is looking very closely at the value of real time information on individual doctors’ performances. Speaking at the BMJ Careers and Health Foundation’s conference earlier this year, the chief clinical information officer at the NHS said that doctors should be provided with their own personal dashboard, including details of the cumulative outcomes for all their patients.The system would be only accessible by the individual doctor. There are many barriers technically and emotionally to getting a system like this running, but from a personal development and learning point of view it would likely be revolutionary. Compare that to the newest RACGP Self Reflection Program initiative.
Learning and development will be cheaper with digital platforms sharing information
Free, is a founding value of FOAMed and it is important to more forward-thinking groups like GPDU and SMACC. Currently medical education is stuck in a paradigm where the College and other commercial providers impose on busy doctor experts to provide them content for free and then they monetise that content for their own organisations. The RACGP monetises access and monitoring, which given the utility of open access platforms today is largely not required. But this activity generates lots of revenue and revenue is seductive. The future is a lot less of this sort of activity facilitated by free sharing platforms, which should be good for everyone, except the private medical education providers, and the odd empire-builder in the colleges.
Hints:
• The RACGP is the major GP learning, training and governance service provider. It is beholden to you, not you to it, and as a vital element of most GPs working lives GPs need to collectively help move the organisation to more modern delivery of services and systems.
• Social media is OK. Try it. It isn’t complex or hard and it won’t bite you. You don’t have to use it at home. But at work, everyone will at least be using it to advance their knowledge and learning. If you’re not on GPDU, give it a go and see what you think.
• You are paying too much for your CPD. It can be done cheaper and better. Be proactive about this as the more efficient your CPD, and the less you spend on it, the more time you will have with patients.
6. Funding and income
This feels like the most out-there prediction. But the logic is there. GPs’ income will improve significantly, both relative to the last decade (which won’t be hard) but more significantly, relative to their more well-remunerated specialist cousins.
But it won’t be easy, and GPs will need to work more smartly and cohesively with government and regulatory bodies to get there.
Here’s how it might work. It will take most of the decade probably.
The majority of very basic GP work is outsourced to a combination of technolog and allied providers, particularly nurses.
This makes being a GP more complex, as both of these downstream resources will need to be managed within the practice. But one factor of taking this on will be more volume at lower cost and higher margin.
GPs will move upstream, not just in the management of chronic care, but in other specialties, made accessible by technology (information, AI telehealth, and connected devices). You will be able to monitor 24 hours for conditions like hypertension, sleep apnoea and cardiac arrhythmias. If GPs don’t adopt the services and technology to do this, which isn’t hard, others will.
Connected devices means more connected patients. It means more services which, to be crude, with technology, are clippable ticket items which makes them convenient and cheap for the patient and more income for the practice.
Telehealth will be a new source of around-the- clock income.
Data will become a source of income, via efficiencies in how GPs work and how they prioritise. But also a lot of other stuff generated on your cloud-based patient management system which will capture all your patient data.
Funding models will shift from volume to data and outcomes.
That’s a controversial call, but the gravity of technology, combined with the desire for better health outcomes for patients, , will drive both the government and the GP sector to move to outcome-based funding.
Hospitals will shrink in size and number as technology enables GPs and other doctors to treat more in smaller decentralised locations. This will bring more revenue opportunity as well.
Hints:
• Medical Homes is in the RACGP vision, but outcomes funding isn’t. That’s a political disconnect that someone will need to address.
• Data about your own performance is gold. The best businesses in the world constantly provide feedback to their people. All confidentially, of course.
• Data is mostly secure on the internet. Think online banking. That’s a pretty big leap already.
• Your local PHN is thinking and implementing a lot of these things. But they are funded differently to you. Perhaps you should get alignment here somehow.
7. Leadership: We’re not in Kansas anymore
Until now, healthcare has largely been spared the stresses seen in other digitally disrupted industries. It’s very hard to accept that it’s going to happen to GPs and make some plans to manage it. Change isn’t something humans like doing. In some ways, the healthcare disruption argument reflects what is being seen in climate change. Is it really happening? What can I do about it anyway? Are we wasting our money preparing for it? Don’t we have a moral obligation (in this case for patients) to do something about it?
Digital disruption has been very slow to come to healthcare. It was held back by the unusual characteristics of the healthcare sector: information asymmetry (power of information to doctors); supply and demand (again, doctors in short supply); risk, governance and regulation (it’s a life and death game).
But disruption is starting to happen now. The good news for GPs is, if you believe any of the above logic, it will be likely good for the profession. It should lead to more interesting and rewarding work, both spiritually and money wise.
It should take the average GP from being mostly alone in a consulting room, to being highly connected with their patients, their peers and their allied healthcare teams. It won’t be good for all doctors though. It is still a significant amount of change to manage.
Leadership and EQ, are going to be the most valuable assets in navigating the change. That is, leadership on an individual level in managing peers, practice, patients and career. And leadership at the level of influencing regulators and the government needs to change faster.
One thing about digital disruption is that the private sector and patients will be empowered to get involved at a much deeper level than has ever hppened before.
GPs are well placed, but they will need to step up, individually and in leading their organisations such as the AMA, the RACGP and ACRRM. They need to be pro-active and get in front of the changes. If they do that, the profession will truly thrive.
References:
1. Harvard Business Review; Oct 11, 2016