The treatment options for scoliosis usually depends on the curve magnitude and the growth potential of the patient
Scoliosis is a curvature of the spinal column in all three planes causing coronal plane deformity (often seen as shoulder imbalance and uneven waist contour), sagittal plane deformity (often seen as loss of thoracic kyphosis and chest wall asymmetry) and rotational deformity in the axis of the spinal column (often seen in the elevation of the scapula or “rib hump”).
Epidemiology
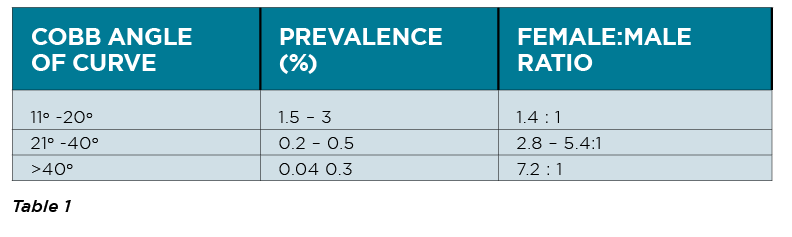
Adolescent idiopathic scoliosis is a common disease with an overall prevalence of 0.5 to 5%. The female-to-male ratio increases substantially with age.
There can be idiopathic and non-idiopathic scoliosis.
Idiopathic scoliosis is further divided into early onset and late onset curves. Non-idiopathic scoliosis can be congenital or neuromuscular/syndromal.
Congenital
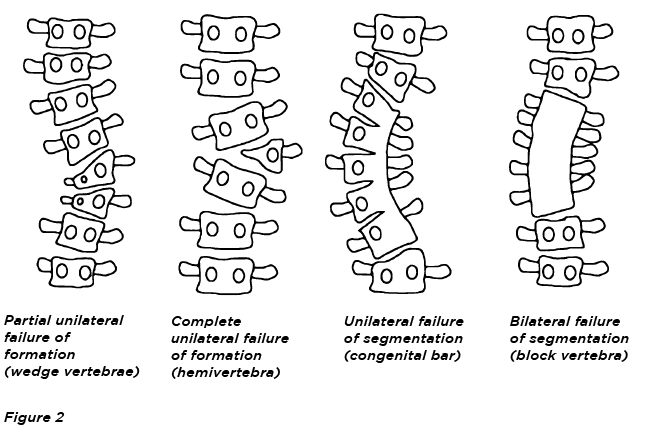
Congenital scoliosis is caused by the malformation of vertebrae like hemivertebra, unilateral bar or block vertebra (See figure 2).
It may not be clinically evident at birth, but the condition will continue to develop until adolescence.
Neuromuscular and syndromic
Neuromuscular scoliosis is caused by insufficiency of active (muscular) stabilisers of the spine in conditions such as in cerebral palsy, spinal muscular atrophy, spina bifida, muscular dystrophies or spinal cord injuries.
Syndromic scoliosis is caused by insufficiency of passive stabilisers of the spine, as seen in Marfan’s syndrome, mucopolysaccharidosis, osteogenesis imperfecta, inflammatory diseases or postoperative after thoracic surgery (open heart surgery).
Early onset
Infantile scoliosis develops at the age of zero to three years and has a prevalence of 1%. Juvenile scoliosis develops at the age of four to 10 years and comprises 10 to 15% of all idiopathic scoliosis in children.
Adolescent
Adolescent scoliosis develops at the age of 11 to 18 years and accounts for approximately 90% of cases of idiopathic scoliosis in children.
Adult
Scoliosis is present in more than 8% in adults over the age of 25, with the prevalence increasing to 68% of people over the age of 60 largely due to degenerative changes in the aging spine.
Prevalence
Genetic factors do influence the incidence and progression of scoliosis. In 97% of cases of adolescent idiopathic scoliosis, there are other family members similarly affected.
AETIOLOGY
The cause of idiopathic scoliosis is unknown. There are different aetiological theories that have been proposed and studied.
Genetic factors
Population studies have shown an increased incidence in families of patients with idiopathic scoliosis compared to the general population. The exact inheritance pattern, genes, and gene products causing scoliosis remain unknown.
Hormonal factors
Melatonin deficiency has been proposed as a cause of scoliosis.
Tissue abnormalities
Several theories have been proposed implicating each structural component of the spine (muscle, bone, ligaments and/or disc) as the causative agent of scoliosis.
Central nervous system theories
Neuromuscular theories are based on the observation that patients with neuromuscular disease often develop scoliosis.
PATHOGENESIS
In adolescent idiopathic scoliosis, the vertebral bodies grow faster than the posterior elements, resulting primarily in a lordosis. The growth forces the bodies to become distorted, that is rotate, in order to create space for themselves. This produces a rotational lordosis. The cause of the unequal growth that is responsible for lordosis is unknown.
DIAGNOSIS
History and presentation
The vast majority of patients with idiopathic scoliosis initially present because they or their family has perceived an asymmetry of the shoulders, waist, or rib cage.
A detailed clinical history should include the following: how the curve was detected, presence of pain, presence of neurological symptoms, any family history of spinal deformity or familial conditions.
A history assessing the growth potential and degree of maturity of the patient is important to estimate their risk of progression of scoliosis. Recent growth spurt, increase in shoe size, development of secondary sexual characteristics (Tanner staging) and, in girls, date of menarche is important.
With congenital spinal deformity attention should be paid to the cardiac, neurological and genitourinary systems.
There are several “red flag” characteristics of scoliosis that suggest the cause may not be idiopathic, and further investigation is warranted:
Approximately 85 to 90% cases of adolescent idiopathic scoliosis involve a right thoracic curve. A thoracic curve convex to the left should raise suspicions of possible additional pathology, including spinal cord tumours, neuromuscular disorders, Arnold-Chiari malformations, or occult syrinx.
Neurological disorders should be considered in patients with neurological deficits or other possible markers of neurological disorders such as midline hairy patches or café au lait lesions.
The clinical examination starts with inspection in the standing position.
Look for asymmetry of the shoulders (specifically look for a difference in height of the AC joints) and prominence of the scapula on one side.
Feel and look for any difference in height of the iliac wing which may indicate a leg length discrepancy that can contribute to the scoliosis. From the front, there may be chest wall asymmetry due to rib deformities. Take note of any skin abnormalities of the skin that may occur along with spinal dysraphism, neurofibromatosis and features of Marfan’s syndrome.
A neurological examination is particularly important as neurological signs often manifest in patients with spinal dysraphism, syringomyelia, Charcot-Marie-Tooth disease and other neurological disorders. Abnormal deep tendon reflexes and/or abdominal reflexes are common in neurological disorders.
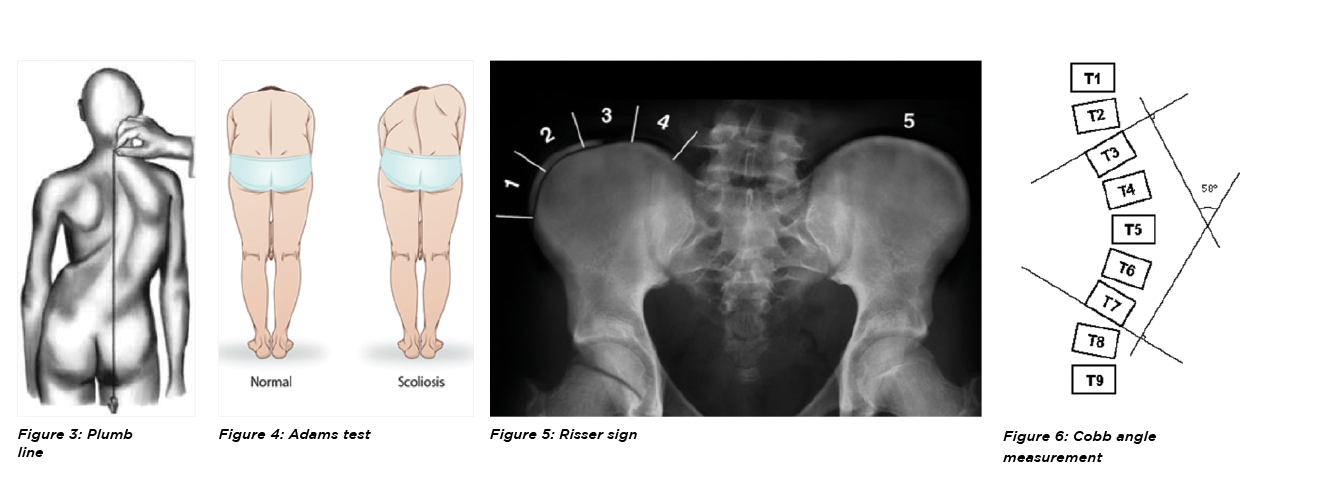
With the patient standing a plumb line dropped from the spinous process of C7 should fall in the gluteal cleft. The distance from this line to the gluteal cleft is a measure of compensation. (See figure 3)
The classic test for structural scoliosis is the Adams Forward Bend Test. The patient bends forward at the waist, standing feet together and knees straight. The patient’s arms hang from the shoulders with their palms together.
The effect of forward bending on the curve should be noted. A “rib hump” will appear with a structural scoliosis on the side of the curve convexity. (See figure 4)
Observing the patient sitting and facing away from examiner is useful to differentiate between a structural and functional (postural) curve. A postural curve improves in the sitting position.
A curve due primarily to pelvic obliquity (or leg length discrepancy) will also improve.
INVESTIGATIONS
Plain X-rays
These should include standing PA and lateral views of the entire spine including the pelvis, on a single film. This allows for evaluation of the iliac apophysis (also known as the Risser sign) and triradiate cartilage in order to calculate bone age and estimate remaining growth potential. (See figure 5)
On PA X-rays, Cobb angle measurements should be made for all major and minor curvatures. Cobb angles are measured by determining the most tilted vertebrae at the cranial and caudal end of each curve. (See figure 6)
An MRI scan of the entire spine and brainstem is recommended in cases where intraspinal pathology (e.g.syringomyelia, Arnold-Chiari malformation, intramedullary tumour/mass) is suspected or at least, needs to be excluded prior to surgical intervention.
PROGNOSIS AND PROGRESSION
The three major factors that determine whether scoliosis will progress are:
patient gender
magnitude of curve on presentation
growth potential
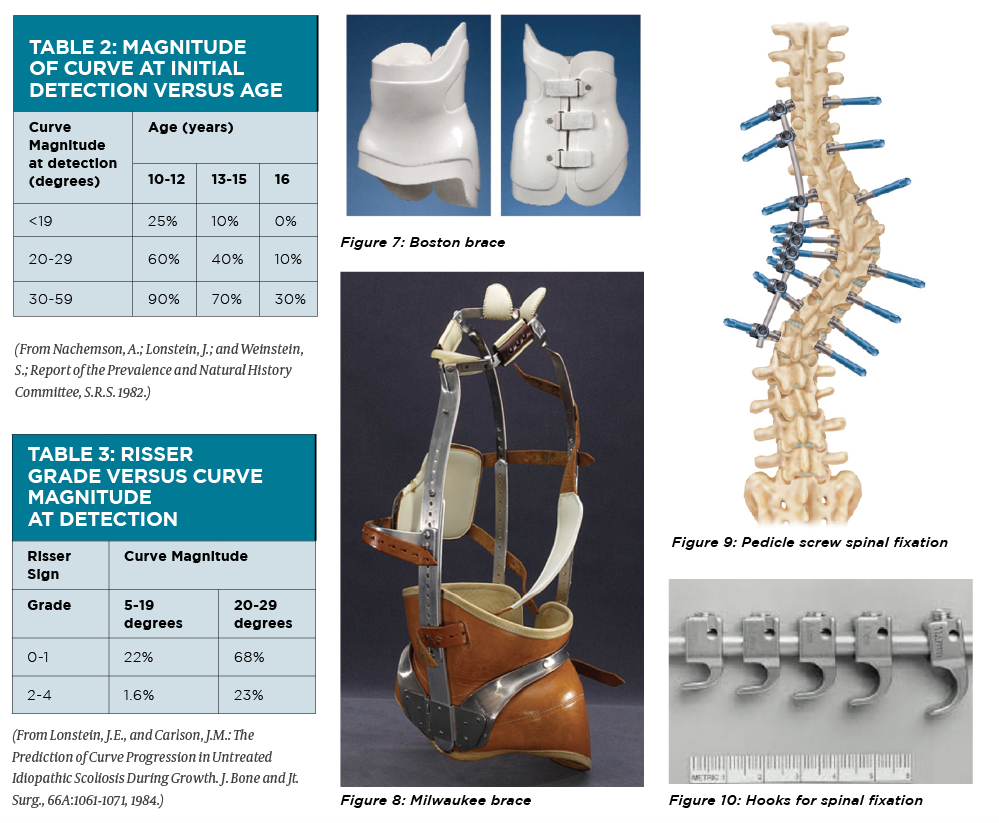
Several studies (See table 1) indicate that scoliosis progresses to a greater severity in girls. Among those patients who have curves greater than 30 degrees, the prevalence ratio of girls to boys can be as high as 10:1.
One study has shown that a Cobb angle of 25 degrees at initial presentation is an important threshold magnitude for long-term curve progression.
The time of greatest curve change is in early adolescence (curve acceleration phase). Prior to the curve acceleration phase progression of the scoliosis curve averages 0.2 degrees per month. Once this phase starts, curves can change 1 to 2 degrees per month.
MANAGEMENT
The management options for scoliosis depend on the curve magnitude and the growth potential of the patient.
Patients with curves greater than 25 degrees are considered for bracing while those with curves greater than 40 degrees are considered for surgical intervention.
Curves that are less than 25 degrees, where the patient is close to the end of their growth potential are generally just observed and monitored with plain radiographs until skeletal maturity.
Non-surgical
Non-surgical management of scoliosis has largely consisted of bracing.
In 1972, Marion “Bill” Miller, CPO, and John Hall, MD, designed the Boston brace at Boston Children’s Hospital. (See figure 7)
The Milwaukee brace was the first brace widely used for the management of scoliosis. Its use for management of scoliosis has largely been replaced by the Thoracic Lumbar Sacral Orthosis (TLSO). (See figure 8)
The TLSO is easy to hide under clothing and fairly well accepted by most patients.
The SpineCor brace (The Spine Corporation) is a nonrigid spinal orthosis which consists of a series of straps.
Data regarding the efficacy of the different types of braces is mixed with differing inclusion criteria preventing direct comparisons.
The Schroth method is a system of exercises that was initially described in the 1920s by Katharina Schroth and further developed by her daughter, Christa Lehnert-Schroth.
The program includes daily exercises and postural control of scoliosis during activities of daily living.
A Cochrane review concluded that only low-quality evidence existed to support the use of exercise programs as a means of treatment for scoliosis.
SURGICAL MANAGEMENT AND FUTURE TRENDS
Posterior fusion with instrumentation is a standard surgical treatment for scoliosis.
Curves larger than 50 degrees progress even after skeletal maturity. In one study curves larger than 55 degrees at skeletal maturity progressed at a rate of more than 0.5 degrees per year.
Curves of greater magnitude inhibit pulmonary function, and much larger curves can cause respiratory failure. Vital capacity below 45% predicted and a Cobb angle greater than 110 degrees are risk factors for developing respiratory failure and early death.
It is preferable to operate before scoliosis patients progress to developing curves of such large magnitudes, as surgery at this late stage is usually more complex and associated with a much higher surgical complication rate.
Posterior instrumentation
Posterior fusion with instrumentation has been a standard of the surgical treatment for scoliosis since first introduced by Paul Harrington.
In the second generation instrumentation system developed by Cotrel and Dubousset, correction was attempted by the rod-rotation manoeuvre.
In modern instrumentation systems, more anchors are used to connect the rod and the spine, resulting in better correction and less frequent implant failures.
Segmental pedicle screw constructs (See figure 9) or hybrid constructs using pedicle screws, hooks, and wires (See figure 10) are the trend today.
Generally, an extent of fusion level is determined with the flexibility of the curves demonstrated on the radiographs taken in supine side bending, fulcrum side bending, traction, or push-prone position.
Anterior instrumentation
Anterior instrumentation surgery was previously the treatment of choice for thoracolumbar and lumbar scoliosis.
However initial enthusiasm for this surgery has waned because of the risk to the thoracic aorta if the screw penetrated the cortex on the opposite side, and the potential to affect pulmonary function following surgical disruption of the chest cage.
Fusionless surgery
Fusion surgery in very young age results in a short trunk relative to the extremities.
It also affects the development of the lung. To provide correction and maintain it during the growing years while allowing spinal growth for early onset scoliosis, the technique of instrumentation without fusion or with limited fusion has been developed. Such fusion-avoiding techniques that are being trialled include anterior vertebral stapling or tethering.
Another possibility being explored is epiphysiodesis on the convex side of the deformity with or without instrumentation. This technique provides a gradual progressive correction, arresting the deterioration of the curves.
However, both these procedures still involve access to the thorax and can lead to a decrease in lung function.
Newer technology is now available to allow insertion of rods that can be magnetically lengthened from outside the body, thus eliminating the need for a general anaesthetic to open the wound every six months to lengthen the rod.
Dr Brian Hsu is an adult and paediatric spine surgeon based in Sydney. His interests lie in all aspects of spine surgery and spinal disorders, in particular, adult and paediatric spine deformity, complex cervical reconstructions, spinal osteotomies and degenerative cervical and lumbar conditions.