Biologics are changing the future for patients with this common skin disease
Psoriasis is a common inflammatory skin disease affecting about 2.3% of the Australian population which means that more than half a million Australians are affected. It can negatively impact patients’ daily activities, such as their ability to work and their social and physical interactions.
There is also a significant impact on their quality of life with an increased rate of depression and suicide in psoriatic patients. It was thought for many years to be only a skin disease but it is now known to be associated with several medical conditions. There have been many recent studies that show an association with metabolic syndrome with an increase in the risk of heart disease, myocardial infarction and stroke. This is because the inflammation is not only in the skin but also in blood vessels leading to atherosclerosis.
Patients with psoriasis are more likely to be obese and have associated high blood pressure, diabetes and elevated cholesterol compared with the general population. These factors need to be considered when treating a psoriatic patient, with clinicians advising on lifestyle issues, obesity, hypertension and smoking in addition to prescribing specific psoriasis treatment.
There have been major advances in knowledge of the immunopathogenesis of psoriasis which is thought to be an autoimmune disorder.
Specific T-cell activation is dependent on innate immune mechanisms and highly specific patterns of cytokines including IL-23. Once the innate immune system has been stimulated, be it through environmental triggers, injury or infection, dendritic cells are activated and produce cytokines including IL-12, IL-23 and others. These cytokines cause T-cell differentiation into Th-1 and Th 17 T-cells which produce Th1- and Th 17 related molecules, particularly IL-17 which stimulate keratinocyte proliferation, further cytokine production including TNF alpha and an influx of neutrophils which results in a psoriatic plaque. The current biologics target these cytokines specifically.
There are several different types of psoriasis with the most common being plaque psoriasis, which typically features the silvery scale and deep erythema which is characteristic of the disease. This psoriasis type, usually begins between the ages of 15 and 40 and develops as a chronic disease that responds to treatment but recurs when treatment is ceased.
Another variety of psoriasis, guttate psoriasis usually occurs after a streptococcal throat infection with an extensive distribution over the body. However, unlike plaque psoriasis, the plaques of guttate psoriasis are small and thin and respond well to treatment usually topical creams or UVB.
There is also a significant impact on their quality of life with an increased rate of depression and suicide in psoriatic patients.
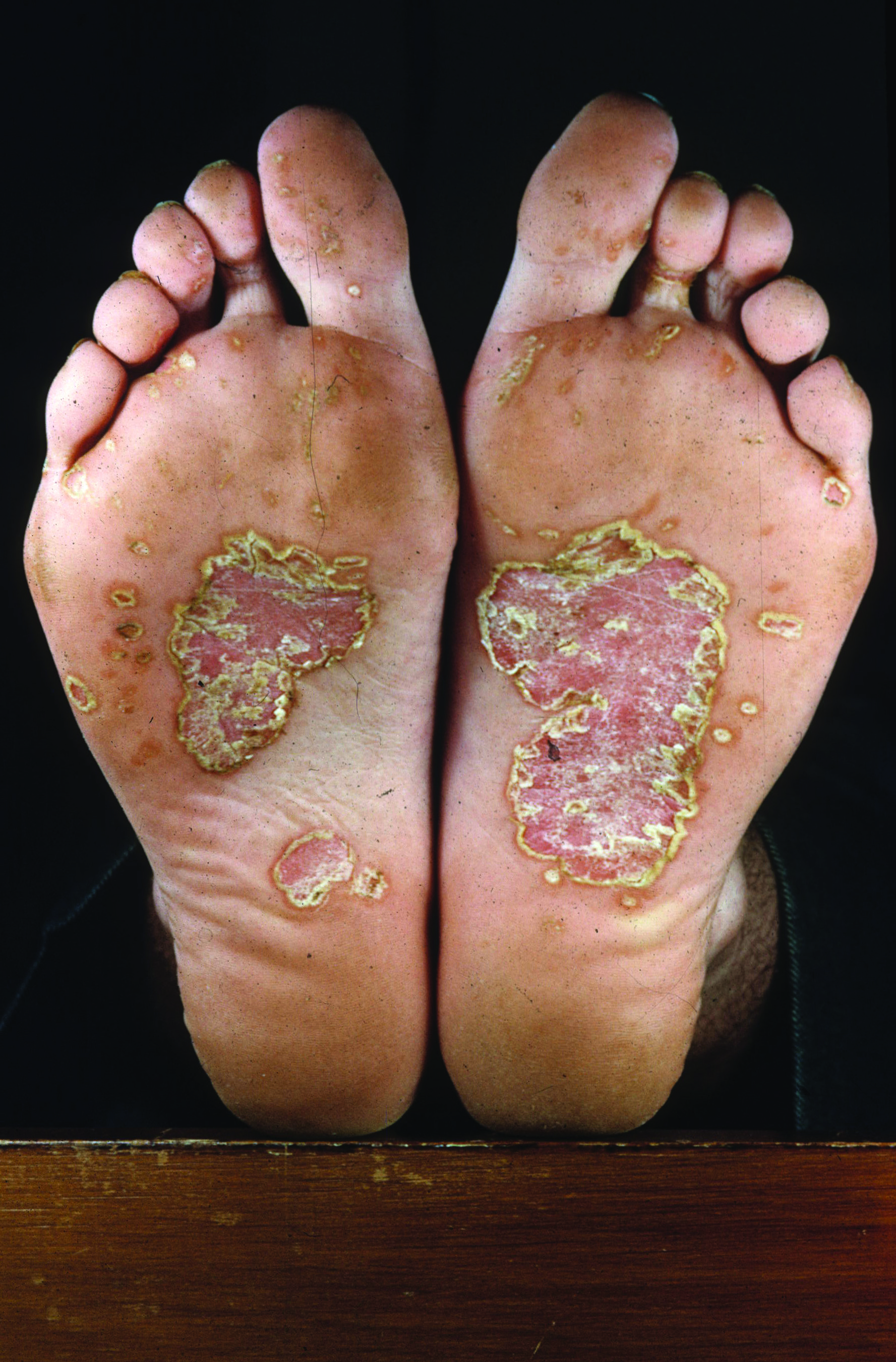
Pustular psoriasis is a less common variety of this condition and there are two main forms. One is localised to the hands and feet and the other is a more generalised psoriasis with erythema and multiple pustules. These patients can be systemically unwell and may need admission to hospital. Pustular psoriasis is a different disease than plaque psoriasis and has different genetic HLA antigens although treatment is commonly the same. Rarely psoriasis may present as erythroderma.
Psoriasis may occur in specific areas such as the scalp, where it is often very itchy, nails, flexural sites, genitalia and a hyperkeratotic form on the hands and feet. Depending on the site and the severity of the skin manifestations of the disease, psoriasis can cause significant embarrassment and disability, affecting a person’s employment, social and personal relationship opportunities.
Exacerbations of psoriasis are commonly triggered by stress although in 50% there is no obvious precipitating event. Other potential triggers include drugs such as hydroxychloroquine, lithium, systemic glucocorticoids, interferons, beta blockers and ACE inhibitors, as well as pregnancy and infection. Smoking is associated with a poor response to treatment. There are no dietary factors that have been shown to help or flare psoriasis however for patients who are obese, losing weight has been shown to improve psoriasis even in the absence of any other interventions.
Psoriatic arthritis is associated with this condition. It occurs in about 30% of cases, and is often not present when the skin disease first manifests but develops over time.
It is important to ask for a history of arthritis especially asking for history of swollen or sausage-shaped digits, morning stiffness, Achilles tendon pain and joint inflammation.
The most common manifestation of psoriatic arthritis is distal interphalangeal joint disease which is often associated with nail involvement in the corresponding digit.
Psoriasis may be associated with other autoimmune diseases such as Crohn’s disease. A person with Crohn’s disease is six times more likely to have psoriasis than a healthy patient.
The management of psoriasis has changed dramatically over the last 10-15 years with the arrival of biologic treatments. They have enabled almost all patients with psoriasis to have much better control and in many cases, complete clearance with few side effects.
The first biologic available for this condition was efalizumab (Raptiva) which was withdrawn from the market after a few years because of a few cases of progressive multifocal leukoencephalopathy, a brain infection caused by reactivation of latent JC virus infection. Efalizumab bound to the CD11a subunit of lymphocyte function-associated antigen 1 and inhibited lymphocyte activation and cell migration out of blood vessels into tissues.
The TNF blockers were the next class of biologics to be used in the treatment of psoriasis and included etanercept, adalimumab and infliximab.
Infliximab has been the most effective TNF blocker but needs to be given by an IV infusion so it is reserved for the more severe and rapidly progressive cases of psoriasis. It is also given on a weight basis of 5mg/kg so it is still effective in obese patients.
The IL 12 and IL 23 inhibitor, ustekinumab, was the next biologic developed and has showed increased efficacy with three-monthly, subcutaneous injections which most patients find very convenient. It is also weight based with 45mg given if under 100kg and 90mg if above 100kg.
More recently the IL 17 inhibitors, secukinumab and ixekizumab have become available. After an induction regime, these biologics are given as a once-monthly subcutaneous injection.
The effectiveness of the biologics have progressively improved.
Initially the aim was to achieve a PASI 75 response which was a PBS requirement to allow continuation of the treatment with these agents. PASI or Psoriasis Area Severity Index is a measure of the severity of psoriasis taking into account the body surface area and the degree of erythema, thickness and scaling. Initial results with the biologics were a PASI 75 response of 40-50% but the most recent biologics are achieving response rates in the order of between 80 to 90%. There are now a significant number of patients on biologics achieving PASI 90 or PASI 100 (clear) responses. The latest biologics are achieving a PASI 100 or total clearance in 40%.
The majority of patients with severe psoriasis can be treated with a biologic and achieve excellent results. The PBS requirements continue to be restrictive and are more strict than other countries where a PASI of 10 or greater is acceptable with other measures such as the Dermatology Quality of Life Index (DLQI) and body surface area greater than 10% are used. In Australia, a PASI greater than 15 is needed before being able to access a biologic as well as a failure to respond to three of four systemic treatments which include methotrexate, acitretin, UVB and cyclosporine.
Patients who are in the moderate category of severity, who do not qualify for a biologic may be more difficult to treat. First line systemic treatments include UVB phototherapy and methotrexate. If patients fail to respond or are unable to tolerate these treatments, second line options, such as acitretin and cyclosporine are available.
Cyclosporine can be very effective but has a high incidence of side effects especially when taken long term (for greater than two years) with hypertension and renal impairment the main concerns. Acitretin works well in a smaller number of patients but the mucocutaneous side effects can be limiting such as dry lips, skin, eyes and nose, headaches, myalgia and hair loss. There can also be elevation of serum lipids, especially triglycerides, and abnormal LFTs.
There are now a significant number of patients on biologics achieving PASI 90 or PASI 100 (clear) responses.
Apremilast is a new treatment which has been approved by the TGA for psoriasis and psoriatic arthritis but is not yet on the PBS. It is a phosphodiesterase inhibitor and is a small molecule given orally. It is an alternative to the current systemic treatments of methotrexate, acitretin and cyclosporine.
It has similar efficacy to methotrexate but does not need regular monitoring with blood tests. The main side effects are nausea, headaches and diarrhoea which usually resolve after the first month. An initial titration regimen is used to minimise these side effects starting at a low dose of 10mg day and increasing to the regular dose of 30 mg twice daily. Many dermatologists have several patients on a patient familiarisation scheme in anticipation of its listing on the PBS, which hopefully will be in the next 12 months.
There are newer treatments on the horizon including biologics that inhibit the p 19 sub unit of IL 23 but do not affect IL 12. These IL 23 inhibitors appear to have similar efficacy to the IL 17 blockers and to date, studies show very promising results. There are also newer small molecules such as the JAK kinase inhibitors which are already on the PBS for rheumatoid arthritis but are showing promising results for psoriasis and psoriatic arthritis.
Patients with more limited disease will still have topical treatment as first line. Topical treatment includes steroids, calcipotriol and the calcipotriol/betamethasone dipropionate combination (Daivobet).
Tar preparations can be helpful in some cases especially for scalp psoriasis but are less cosmetically acceptable and are not used often. Dithranol is still used in day-patient treatment centres but because of the high risk of staining and irritation is not used much at home but still has a place. There is a new topical treatment of calcipotriene/ betamethasone dipropionate (Enstilar) which is a foam formulation of Daivobet.
The foam formulation is more acceptable to the patient and there is increased penetration of the active ingredients and increased efficacy with this formulation. There are also topical formulations of phosphodiesterase inhibitors and JAK kinase inhibitors being developed.
It is an exciting time to be involved in the treatment of psoriasis with many new and effective treatments especially for severe cases. Nonetheless, the psoriasis patient still needs to be treated holistically with attention to lifestyle factors and reduction of risk factors for metabolic disease.
Dr Warren Weightman is the Head of Dermatology at Queen Elizabeth Hospital, Adelaide