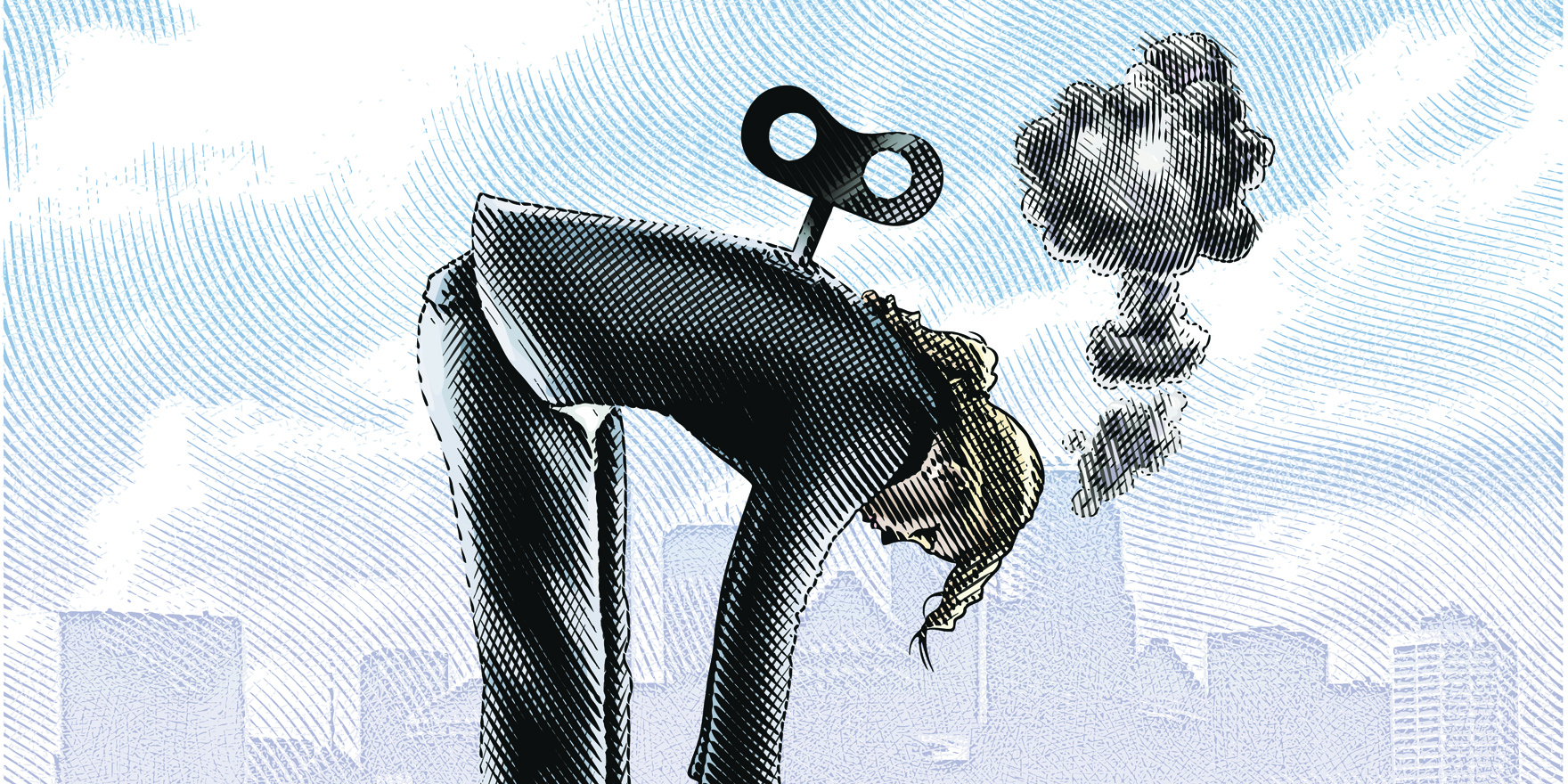
Strategies to combat burnout focus on doctor resilience rather than the system processes that underpin the stress
General practice is suffering from a grieving workforce, and efforts to combat burnout by increasing resilience may be counterproductive, according to a US family physician.
“Physicians have traditionally encountered losses – regularly confronting death in the context of the care of their patients,” Dr Deborah Lathrop wrote in the Annals of Family Medicine this month.
“They may not, however, recognise that they are surrounded by more ambiguous losses, including rapidly changing expectations of their duties, roles and regard.”
The last two decades have seen major changes to doctors’ workplaces, including the shift away from running private practices to becoming employees, the growing burden of paperwork and regulation, electronic health records, and changing credentialling demands.
For example, a doctor might feel their sense of professional integrity threated by their perceived inability to deliver care at an acceptable pace, when squeezed in by other stakeholders to get through more patients, Dr Lathrop said.
“These changes, while incremental, have been continuous and taken en masse, have required adjustments in how we practice medicine,” Dr Lathrop said.
“These adaptations incur loss.”
Dr Lathrop points to the definition of disenfranchised grief as “grief that persons experience when they incur a loss that is not, or cannot be, openly acknowledged, publicly mourned or socially supported”.
Physicians might also avoid acknowledging the impact of these changes, further complicating the experience of grieving, she said.
“For those lamenting, even on an inexplicit level, grieving drains one’s physical energy, emotional stamina, and, at times, intellectual capability,” she wrote.
“Grieving, therefore, both at work and because of work, could contribute to what we typically define as risk factors for professional burnout.”
Burnout was prevalent, affecting between one third and one half of the doctor workforce.
However, strategies to combat burnout had traditionally focused on doctors themselves and improving their stress levels and resilience.
But the evidence did not back up techniques such as stress reduction and mindfulness in combating this burnout. However, evidence did point to system processes as underpinning burnout, she said.
“This approach erroneously implies too little resilience or a weakness within the physician, while diminishing or even exonerating the healthcare delivery apparatus and organisations in which physicians’ work.
“In so doing, the physicians’ grief, and suffering, is disenfranchised by the system.”
Additionally, because there was a long period between training in medical school and being able to work independently, “dissonance may develop between the expected role and regard a physician held before entering the profession versus one’s current experience”.
“Suffering physicians could benefit when they acknowledge [that] changes in their work environment incur loss, chose to address any pain from hidden grief, withdraw emotional energy from earlier professional expectations, and reframe their professional future.
“For example, there is a role adjustment required for physicians to go from being the holder of unique knowledge, to that of an expert partner, aiding patients through internet-mediated doctoring.” A manifestation of this was the introduction of the term “provider”, which lumps doctors in with a whole range of other healthcare professionals. This shifted the identification from the title of doctor, which embodied the hard-sought training, ethical mandates and knowledge-based authority, to the service they provide, she said.
“In these ways physicians receive conflicting and/or marginalising messages, which results in a loss of occupational esteem, and can evoke internal dissonance.”
But recognising the impact of grief in the profession also offered solutions.
Doctors treating other doctors could name and validate the loss they were feeling, educators could prepare future doctors for the evolution their job would undergo, and doctors in leadership roles could bring awareness of the way organisational changes could impact on doctors’ inner work life, Dr Lathrop said.