The vast majority of people with a recorded penicillin allergy aren’t actually allergic to these antibiotics, US research shows
US researchers are urging doctors to double check their patients’ penicillin allergy status, as more that 95% of people with recorded penicillin allergy can tolerate this class of antibiotics.
Around 9% of Australians go through life avoiding penicillin because of a note in their medical record says they’re allergic, but only a tiny minority of these actually have clinically significant reactions to the drug.
Often, patients were inappropriately prescribed penicillin for a virus as a child and the subsequent rash was misinterpreted as a penicillin allergy.
Being cut off from access to penicillin for life due to a false allergy label was a handicap for many patients, researchers at the Infection Control Unit at Massachusetts General Hospital in Boston wrote in a JAMA paper this month.
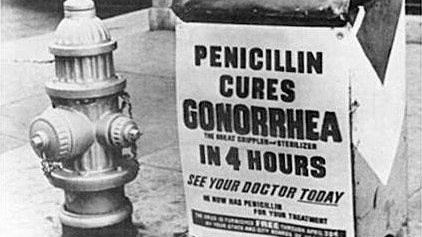
Penicillins were a fairly low-cost, first-line treatment for many infections, such as UTIs, syphilis and gonorrhoea.
The alternatives to penicillin were usually more expensive, more toxic and could raise the patient’s risk of developing Clostridium difficile, the authors said.
The solution was to test whether patients actually had an allergy to penicillin. After taking a thorough history, low-risk patients could be given an amoxicillin challenge either as a prescription or under observation, while moderate-risk patients could undergo a skin test followed by amoxicillin challenge, the authors said.
Patients who had a penicillin allergy as a child could be re-tested, as around 80% of patients became tolerant after a decade.
Penicillin desensitisation (where patients were given increasing amounts of the allergen) should be reserved for the minority of patients with severe reactions and a positive skin test, the authors said. A patient with a negative skin test was very unlikely to have an allergic reaction to penicillin in the future.
The alternatives to penicillin, such as fluoroquinolones and vancomycin, were a greater contributor to antibiotic resistance than penicillins, increasing the risk of methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus.
“All of these drugs encourage antimicrobial resistance, but one of the principles of appropriate antibiotic use is using the most narrow spectrum of antibiotics that you can,” Dr Evan Ackermann, a GP on the Gold Coast in Queensland, said.
“With the antimicrobial stewardship becoming more prominent, there’s a role now to properly test people to understand their true allergic status,” he said. “We do need a process where it’s fairly simple and straight-forward and can be undertaken by general practice easily.”