The steroid dexamethasone can be considered for the treatment of adults with COVID-19 who are receiving respiratory support, including those on mechanical ventilation, according to latest Australian guidelines update
Welcome to Friday on The Medical Republic‘s live COVID-19 blog.
Got any tips, comments or feedback? Email me at bianca@biancanogrady.com
The latest
- Afternoon update: Consider dexamethasone in ventilated and oxygenated patients with COVID-19, study finds higher stroke risk with COVID-19 than influenza, and the latest TMR podcast drops.
- Morning update: A returned traveller is NT’s first new case since early May, New York researchers report more on paediatric multisystem inflammatory syndrome, and 40% of cases in long-term aged care study are asymptomatic.
- The steroid dexamethasone can be considered for the treatment of adults with COVID-19 who are receiving respiratory support, including those on mechanical ventilation, according to the latest update from the Australian National COVID-19 Clinical Trials Taskforce.
The advice suggested 6 mg of daily intravenous or oral dexamethasone for up to 10 days, but advised against using it in patients who do not require oxygen. The update is based on the findings of the UK-based RECOVERY trial, which suggest a reduction in mortality rates among ventilated patients and those on oxygen. - COVID-19 may be associated with a higher risk of stroke, according to a study which compared stroke rates in patients with COVID-19 and those with influenza.
The retrospective cohort study of 1916 COVID-19 patients and 1486 patients with influenza, published in JAMA Neurology, suggested individuals with COVID-19 had at least a seven-fold greater odds of experiencing stroke, even after adjusting for age, race and sex.
When the authors adjusted for vascular risk factors and intensive care admission, there was still a four-fold greater odds of stroke among those with COVID-19 compared to those with influenza. They also saw significantly higher plasma D-dimer levels in those who experienced stroke compared to those who did not.
“These findings suggest that clinicians should be vigilant for symptoms and signs of acute ischemic stroke in patients with COVID-19 so that time-sensitive interventions, such as thrombolysis and thrombectomy, can be instituted if possible to reduce the burden of long-term disability,” they wrote. - Want to catch up on what’s been happening on the COVID-19 live blog but can’t be bothered reading it? Check out the latest TMR podcast, featuring reporters Felicity Nelson and Francine Crimmins, and COVID-19 live blogger Bianca Nogrady.
- A study in long-term aged care facilities in the United States has found around 40% of those who tested positive for SARS-CoV-2 were asymptomatic.
The study, published in Emerging Infectious Diseases, screened 938 residents and staff of nine facilities which had recorded at least three positive tests already. It found the overall prevalence of SARS-CoV-2 infection was 70% using RT-PCR testing, and female residents had a slightly higher rate of asymptomatic infection than male residents.
“Because the potential for asymptomatic transmission of SARS-CoV-2 is concerning, for greater effectiveness, infection control efforts in LTCFs [long-term care facilities] should include both mass testing–based strategies and symptom screening,” the authors wrote. - A network of New York hospitals has reported 99 cases of so-called ‘multisystem inflammatory syndrome’ in children since the start of the COVID-19 pandemic. The syndrome has previously been described as Kawasaki’s or Kawasaki-like disease, toxic shock syndrome or myocarditis.
The children presented with symptoms such as fever, hypotension or shock, severe cardiac illness or other severe end-organ illness, rash, conjunctivitis, skin or gastrointestinal features, according to a paper published in NEJM.
Of the 99% who were tested for SARS-CoV-2 using RT-PCR, only one in five tested positive. Of the 81% who were tested for antibodies, 47% were positive. However all but one of the 77 patients who were tested for the presence of IgG antibodies to SARS-CoV-2 came up positive.
Four-fifths of the patients were admitted to intensive care, and ten received mechanical ventilation. Two children died, possibly from complications of inflammatory, coagulopathic or neurological nature.
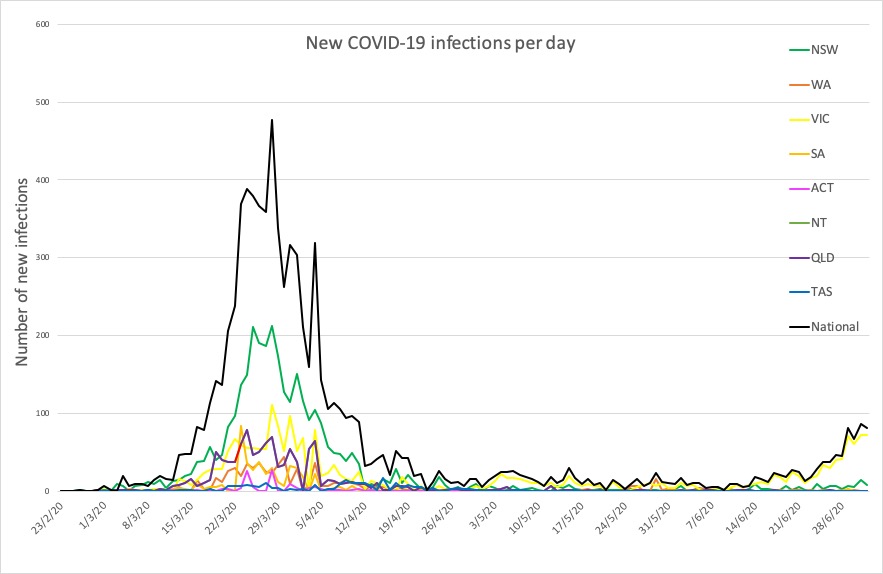
The authors noted that this condition appeared to affect children from all racial and ethnic backgrounds, and called for surveillance for potential cases of multisystem inflammatory syndrome, particularly in communities with a higher prevalence of COVID-19. - Northern Territory has recorded its first new case of COVID-19 since early May; a returned traveller who flew to Darwin via Brisbane and Melbourne. Case numbers continue to rise in Victoria with 77 new cases recorded yesterday (and five previous cases reclassified as negative), all acquired within the state.
The Sydney suburb of Balmain is on alert after a worker at Balmain Woolworths tested positive, and NSW Health is urging anyone in the area with symptoms to get tested.
The worker had actually been in hotel quarantine in Melbourne for two weeks after returning from overseas, according to a statement from NSW Health. He had developed symptoms while in quarantine, tested positive on day 7 of quarantine, but was released on day 14 of quarantine. He then flew to Sydney, and after working at Woolworths, then presented with symptoms again, was tested again and found to be positive. Store staff have been told to self-isolate.
Here are the latest confirmed COVID-19 infection figures around Australia to 9pm yesterday:
National – 8001, with 104 deaths and 7090 recovered
ACT – 108
NSW – 3211
NT – 30
QLD – 1067
SA – 443
TAS – 228
VIC – 2303
WA – 611