A cohort study of 217 critically ill COVID-19 patients admitted to intensive care in three acute-care hospitals in the United States has recorded an overall mortality rate of around 25%.
That’s a wrap for The Medical Republic‘s live COVID-19 blog.
Thanks to our sponsor and supporter for funding this project with an independent grant, Boehringer Ingelheim.
The latest
- Mortality rate of 25% in COVID-19 patients admitted to ICU in the US.
- Contact tracing shortens the time to diagnosis by more than two days, and time to isolation by nearly two days.
- Is full PPE enough? Study suggests viral particles can still get on skin, hair and clothes.
- A cohort study of 217 critically ill COVID-19 patients admitted to intensive care in three acute-care hospitals in the United States has recorded an overall mortality rate of around 25%, according to a non-peer-reviewed study published on MedRxiv.
Three-quarters of the participants received invasive mechanical ventilation and four patients received extracorporeal membrane oxygenation.
Nearly 60% of the cohort were transferred alive from the ICU, around one-quarter died in the ICU and 40% survived to be discharged from hospital. However 16% were still in the ICU at the end of the study, and more than a third of these were still on mechanical ventilation. Among those who were ventilated, the mortality rate was just over 28%. The median stay in ICU was 12 days.
The study found that patients who died had a significantly higher Sequential Organ Failure Assessment score on admission to the ICU, and median D-dimer values among those who died were two times higher than among patients who survived. Patients who died were also more likely to have respiratory failure and experience shock that required treatment with vasopressors.
The authors commented that the mortality rates they observed – 25% – were substantially lower than seen in other studies, where they ranged from 50%-97%. They also said the mortality rates among patients who needed invasive mechanical ventilation were lower than those reported elsewhere.
“These data indicate that a majority of critically ill patients with COVID-19 can have good clinical outcomes and support the ongoing use of mechanical ventilation for patients with acute respiratory failure,” they wrote.
However they also acknowledged that their location – the state of Georgia – experienced a later arrival and peak of COVID-19 infections, which gave the state more time to organise and prepare for the pandemic. Their guidelines also emphasise early intubation and lung-protective ventilation strategies.
- Contact tracing of COVID-19 means infected individuals are diagnosed more than two days earlier and isolate nearly two days earlier than they would otherwise, according to a study on contact-based surveillance published in Lancet Infectious Diseases.
Researchers from the Shenzhen Center for Disease Control and Prevention retrospectively examined data from 391 SARS-CoV-2 cases and 1286 close contacts, and found that positive cases isolated on average 4.6 days after developing symptoms, but those who were contracted traced isolated themselves 1.9 days earlier than this.
The secondary infection rate – the rate at which a single case infected others – was around 11% for people in their immediate household, and nearly 7% overall. Travelling with an infected person was associated with a seven-fold higher odds of infection.
The study also found that the rate of secondary infection in children aged under 10 years was similar to that of the population average and the age of the index case didn’t seem to change the secondary infection rate.
Close contacts included people who lived in the same apartment, shared a meal, travelled together or interacted socially with the index case in the two days before symptom onset. It did not include casual contacts or healthcare workers who wore a mask during exposure.
Only 9% of infections were described as ‘severe’, and among the 228 patients where outcomes were known, there were three deaths.
Analysis of 183 cases where there was data on exposure and symptom onset found that the median time between exposure and symptom onset was 4.8 days, with 95% of those who developed symptoms doing so within 14 days. But there were still 5% of patients who did not show symptoms until 14 days after infection.
“This work further supports the understanding of COVID-19 as a disease with a fairly short incubation period (mean 4–6 days) but a long clinical course, with patients taking many weeks to die or recover,” the authors wrote.
- Even with full PPE, healthcare workers may still get SARS-CoV-2 viral particles on their skin, hair and clothing, according to a study which used a fluorescent dye to examine contamination during a simulated intubation exercise.
According to a research letter published in JAMA, Israeli researchers conducted two simulations of patients in respiratory distress needing intubation, using manikins (yes, that is the spelling) – one adult, one child – that were equipped with a device that ‘exhaled’ droplets during coughing episodes. A dye only visible under fluorescent light was used for the droplets.
The two doctors and two nurses in each scenario wore full PPE, including N95 respirators, eye protection, gowns and gloves. However this did not include coveralls, shoe covers or hair coverings.
The study found that after the 20 minute procedures, seven of the eight participants had fluorescent marker on on their exposed skin – six on their neck and one on an area – all had it on their hair and four also had the marker on their shoes.
The study’s authors, while acknowledging this was only a simulation study, said it suggested clothing covering all the skin could diminish the risk of spread.
An accompanying editorial said fundamental research was needed to better inform recommendations about PPE use.
“For example, it would be useful to know how long SARS-CoV-2 can remain infective on surfaces such as the skin, hair, and clothing, and the potential for contact transmission from those sites to guide recommendations for barrier protection,” they wrote.
10.55am, 28 April
- And winner of the Poker Face of the Week award goes to the US Federal Emergency Management Agency, which has a dedicated Coronavirus Rumor Control page addressing such rumours as ‘Is 5G cell phone technology linked to the cause of coronavirus’ and ‘Is FEMA seizing medical supplies’.
Other questions answered include ‘Are there any vaccines to prevent or medicines to treat COVID-19’, and ‘Is the government sending everyone money’.
There’s something familiar about all these rumours … I could have sworn I heard someone on TV saying these things. Just can’t put my finger on who it is.
Also, noticeably absent from the list of rumours being addressed is ‘If I inject disinfectant into my lungs, will this cure me of COVID-19’. Can’t wait for that one.
- The Therapeutic Goods Administration is getting its arse-kicking boots on and going out after anyone breach the code on advertising, sourcing or supplying COVID-19 testing kits. On Friday last week it issued three infringement notices; one for importing test kits not on the Australian Register of Therapeutic Goods, one for making a false or misleading statement about COVID-19 test kits, and one for advertising rapid test kits.
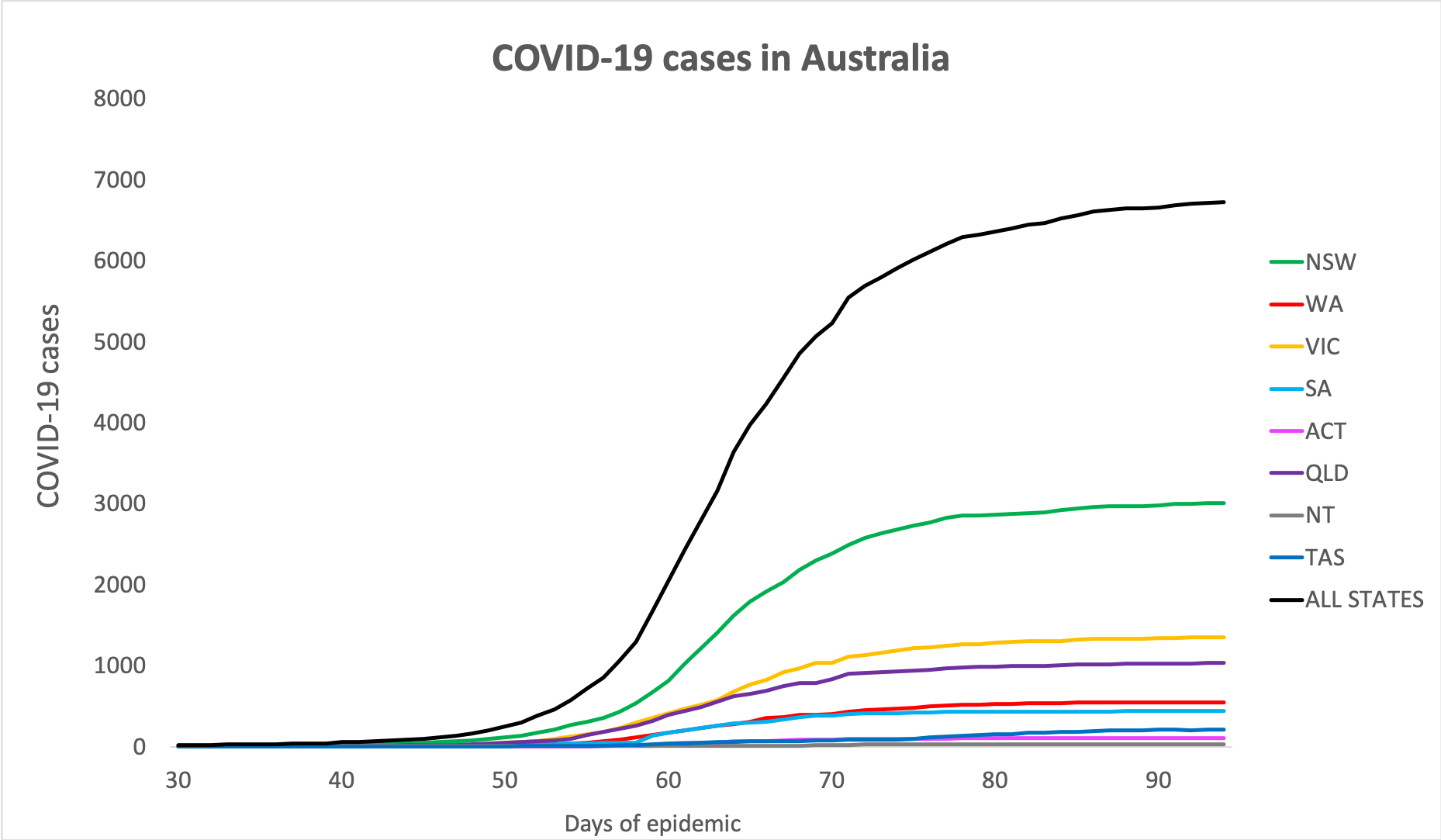
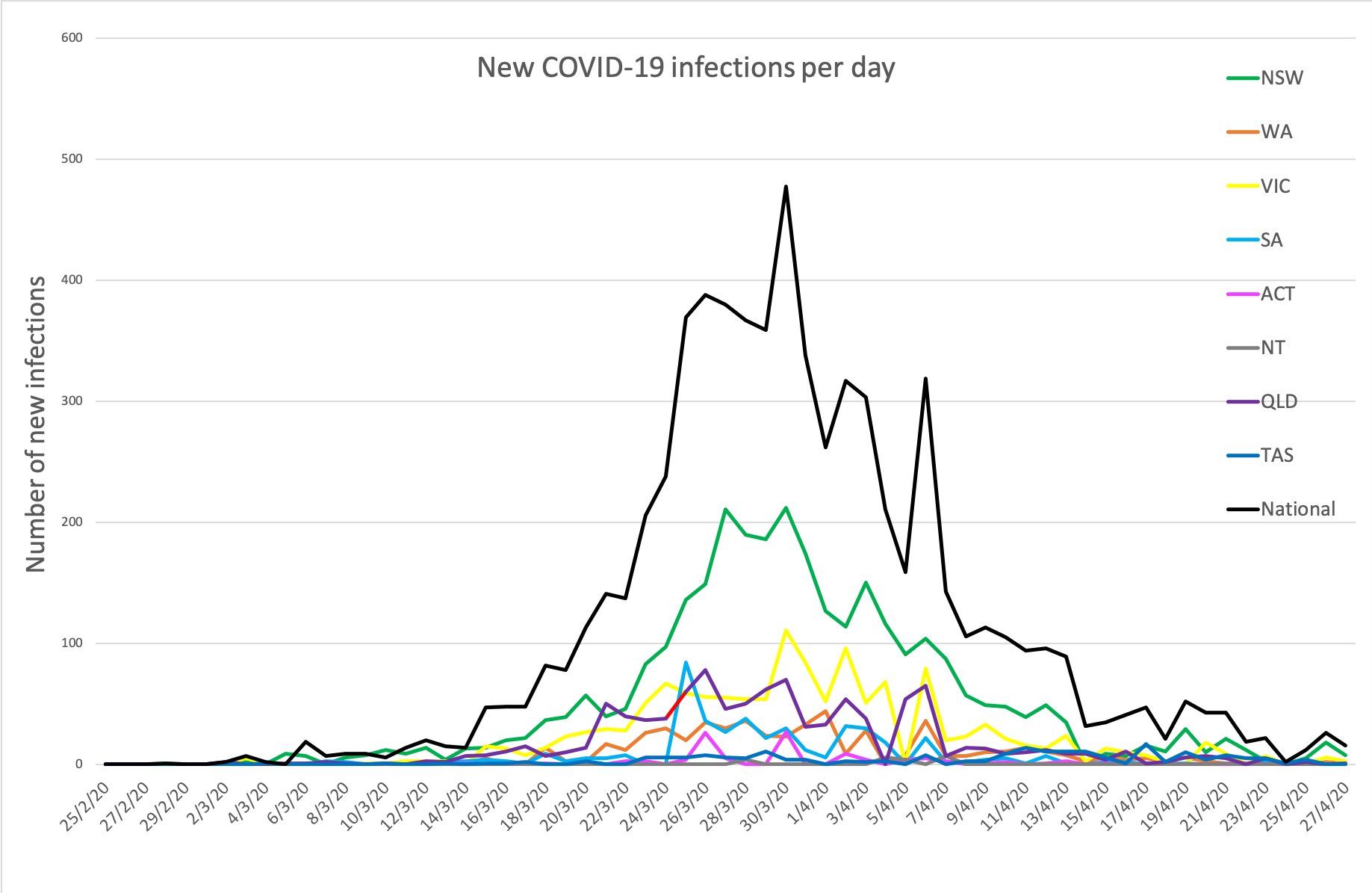
- Here are today’s confirmed COVID-19 infection figures and new infections from around Australia, to 6am this morning. Big thumbs-up to Northern Territory, which has had no new infections for eight days, and South Australia, which has had no new infections for five days:
National – 6725 (up 12), with 84 deaths and 5,602 reported as recovered
ACT – 106
NSW – 3009
NT – 27
QLD – 1033
SA – 438
TAS – 214
VIC – 1349
WA – 549
Disclaimer: The content on the Medical Republic COVID-19 blog is independently created by Medical Republic without input from Boehringer Ingelheim Pty Ltd. The views, information, or opinions expressed on the Medical Republic COVID-19 blog are Medical Republic’s own and do not necessarily represent those of Boehringer Ingelheim Pty Ltd. Boehringer Ingelheim Pty Ltd is not responsible for and does not verify the accuracy of any content on the Medical Republic COVID-19 blog.


