The unintentional racism inherent in the institutions we work in is widespread and insidious, and often hard to notice
I am racist. It’s not that I’ve become friendly with Pauline Hanson recently. I’m not shouting at people on trains, and I’m not longing for a mythical 1950s Australia where the people are as white as the picket fences. In fact, the only views you’ll find me expressing are those fully welcoming of all humanity in its glorious diversity. And yet I am racist. And, I am sorry to say, I suspect you are, too.
Now I know, dear reader, that you are not refusing care to patients on the basis of their skin colour, ethnicity or religion. I trust that you are treating your colleagues of all backgrounds and cultures fairly. However, we know from the research that at least 30% of our Aboriginal and Torres Strait Islander patients say they have experienced racism in the health system. When I talk to my Aboriginal patients, just about every single one has stories of being treated disparagingly, or being shamed and embarrassed by staff attitudes. So widespread is this that the “Close the Gap” campaign has called for a national inquiry into racism in healthcare settings.
Even among our colleagues, we hear of sly comments. I’ve heard from an Australian GP registrar whose family were from China having mocking comments about him made in his practice. I’ve heard of a GP supervisor calling other cultures primitive, not realising the offence he was causing to his registrar.
These examples are just the most blatant, and we will all have come across them. But more subtle than this are the things we do without thinking, just because it’s the way we’ve always spoken.
Think about some of the language we use about international medical graduates as if they (actually, “we” – I trained overseas, too) are all a problem to be solved. We talk as if we all come from that strange country that’s called “overseas”.
The truth is that visiting the various bits of our health system is a stressful experience for many of our patients. Of course, being unwell is stressful, but seeing people who hold these attitudes often adds to the discomfort.
That may not all be due to racism. But our complex health system is set up to be the sort of service in which those setting it up are comfortable. All of our small decisions contribute to this, from the languages displayed on our walls, to the way we use phone and online access instead of face to face, to opening hours, to the way we get away with talking about patients and colleagues.
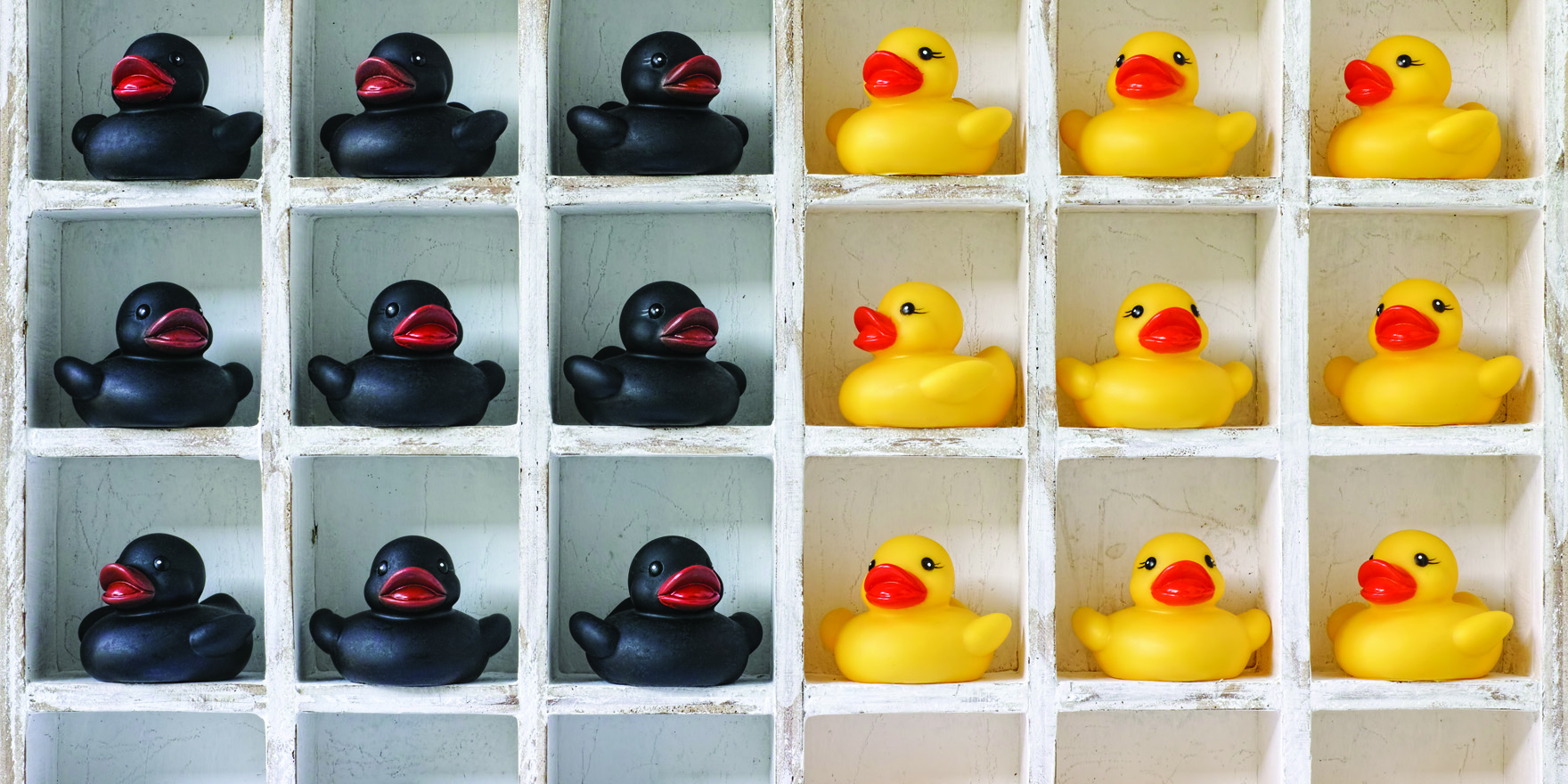
All these small decisions add up to services that are intuitively understood by those in mainstream cultures, but feel unwelcoming to those of other cultures, whether they be Tharawal, Tamil or Thai.
Wherever we’ve seen these barriers overcome, it has started with listening to people from those cultures and taking them seriously, be they patients or staff. What we hear, we act on to change our service. This can result in different posters on the wall and faces behind reception, or services with coffee machines and internet access in the waiting room. I’ve even heard of one surgery that set up as a whisky bar to attract male patients. The common theme, however, is ceding some control to our communities – often a difficult thing for doctors to do.
Which is why I say I’m racist, and why I think you might be, too.
All of us can stand against racist actions where we witness them, especially when it’s from our colleagues.
While racist rants still occur and are easy to condemn, the unintentional racist outcomes of the institutions in which we work are much more widespread and insidious, and correspondingly hard to notice and change, especially for those of us comfortable in the current system.
So how can we be less racist, you and I? Well, we need to acknowledge that our own experiences are not universal. My experience as a straight, white, male doctor means I am not exposed to the racism experienced by doctors of many backgrounds across Australia.
Our experiences and lives as doctors are often different to those of our patients. We are in well-paid work, and have a degree of control over our lives, unlike many of our patients. By virtue of the letters after our name, we have some power in the health system – certainly more than our patients do.
We can all listen closely to our patients – it’s what we’re trained to do, after all – and try to make our bit of the health system more responsive to their needs. All of us can stand against racist actions where we witness them, especially when it’s from our colleagues.
This is especially important for those of us who are more senior in our careers, or who have professional leadership roles in education, academia or with the colleges.
Many GP registrars are concerned that speaking up about racism will lead to problems progressing through training. All of us need to create a professional culture in our services where racism is unacceptable, and we call it out where we see it.
We need our professional bodies to take a stand, and support those who call out racism too. The solutions to institutional racism are institutional, after all.
The RACGP is a signatory to the “Racism: it stops with me” campaign from the Human Rights Commission, and they have resources available to help stand up to racism safely. The charity, All Together Now, also has resources, both for individuals and organisations.
As racism is demonstrably harmful to health, it’s clear that it should form no part of a health system.
When all of our patients can say they can access the health system anywhere they choose, confident that they will be treated well, then I will be happy to say I am not racist.
Dr Tim Senior is a GP working in Aboriginal and Torres Strait Islander health at GP Tharawal Aboriginal Corporation