GPs remain the most cost-effective part of Australia's health system, seeing more patients and providing more services despite stagnant funding
A new report showing federal spending on general practice grew by just 80c per person in the latest year has sparked calls for fresh investment and new models of patient-centred primary care.
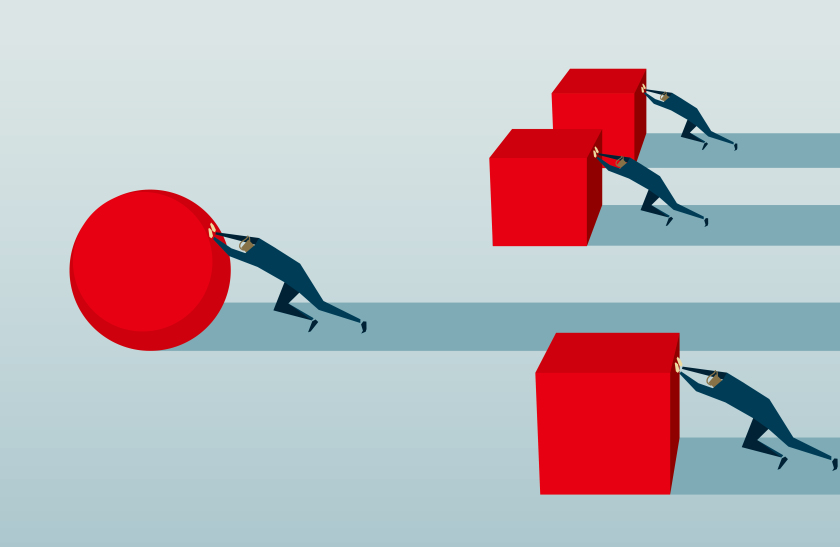
The Productivity Commission’s report on government services confirmed GPs remained the most cost-effective part of the health system, seeing more patients and providing more services despite stagnant funding.
“This highlights the funding pressure that general practice continues to operate under,” AMA President Dr Michael Gannon said, referring to the meagre funding growth.
“A well-resourced general-practice sector can help keep patients out of hospital and save the health system money.”
Federal government spending on general practice in the year to last June edged up from $370.60 to $371.40 per Australian. PBS spending sits at a comparable level, but spending on hospitals exceeds $2500 per person.
Demand for GP services continued to grow in the year, driven by a rise of complex and chronic diseases, the ageing of the society, population growth and improving access to GPs.
On average each Australian used GP services 6.5 times last year, an increase from 5.9 services in 2011-12.
The commission calculated there were 105.9 full-service-equivalent (FSE) GPs per 100,000 head of population in 2016-17, up significantly from 82.9 five years earlier.
Dr Gannon said the report was “compelling evidence” that the government should provide more investment and support in the coming budget.
Consumers Health Forum CEO Leanne Wells said the report exposed the fragmented and ill-fitting nature of health services and a lack of focus to date on containing a massive, growing burden of chronic disease.
She said it was time to ask what mattered for patients and develop better models of primary care.
Work in Australia to prevent and manage chronic disease in primary care was still in its infancy, she said.
“We know Australia generally has a high standard of healthcare, but disconnects within and between services in community and hospital result in less optimal care, particularly for those with chronic and complex conditions as well as waste in the system,” she said.
RACGP President Dr Bastian Seidel said the health system needed to shift focus from expensive treatments in institutions to effective strategies to maintain health within the community.
“GPs and their healthcare teams provide over 150 million patient services at a fraction of the cost of the far more expensive, overcrowded hospital system, yet our government continues to look past them and the value they bring to our community,” he said.
He also urged a rise in the Medicare rebate for longer GP consultations.
“The federal government can really make a difference to the quality of care GPs are able to provide Australians, by increasing this rebate,” he said.
Ms Wells said dysfunctional federal-state health funding arrangements, and the failure of the Medicare system to meet the needs of people with complex and chronic conditions, put up barriers to effective, evidence-based healthcare
“Evidence from around the world shows that ‘people-centred care’ delivers better health outcomes for the individual and better economic results for the community.”