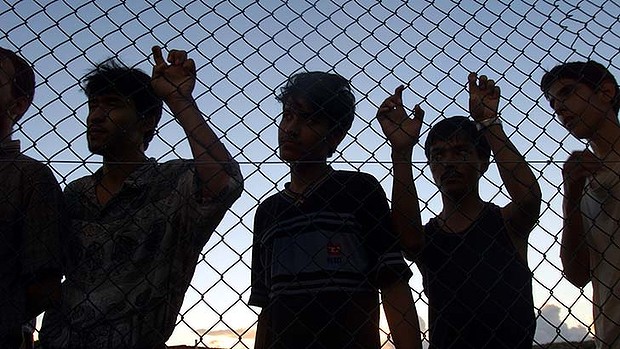
Health professionals have to navigate an ethical minefield working in offshore detention facilities. The crisis on Manus Island is a case in point
As the standoff between hundreds of asylum seekers in the Manus Island detention facility and PNG authorities continues, we are witnessing a potential crisis of health and mental health among these detainees.
As a psychiatrist, I have had direct contact with current Manus detainees who are experiencing increasing anxiety and distress and an uncertain future.
Some of these people are treated with medication, usually antidepressants, and some feel that this provides them with some symptomatic relief. Detainees I’ve spoken with have informed me that medications will no longer be supplied.
There are significant risks associated with sudden withdrawal of medication particularly when facing increased anxiety and stress. In the case of detainees, these withdrawal symptoms could include agitation, depression and a greater risk of suicide or self-harm.
Governments need to seriously consider that the consequences of failure to provide treatment to people under their care are significant and can be seen as gross negligence and human rights abuse.
Endemic problems with offshore detention
Australia’s system of offshore processing of asylum seekers and refugees has been widely criticised both within Australia and internationally since it was first introduced in 2012.
This criticism has often centred on the limited health facilities being offered to detainees and the logistical difficulties in providing expert medical and health staff.
This has led to tension between clinicians and government where health providers recommend as necessary transfer of detainees to appropriate locations to receive treatments. This often leads to disputes with the Australian government who fear that mainland legal challenges to return would be raised.
The pervasive culture of the detention environment has been one of disregard or minimisation of mental suffering among detainees. In some cases detainees have been blamed for their own deterioration – or assumptions made that these are not genuine conditions.
A recently release Human Rights Watch report on refugees on Manus Island highlights longstanding concerns of inadequate heath care, medical neglect and mental deterioration
This situation raises serious questions about the possibility of providing much-needed care in this environment and the way doctors’ ethics and practice are compromised. Outbreaks of riots and self-harm were witnessed with horror as they unfolded in mainland centres during the early period of immigration detention.
The crisis of mass distress in Woomera and Baxter detention centres prompted concerns around the damaging impact of mandatory detention of vulnerable groups and particularly the harm done to children and unaccompanied minors.
Several committees of inquiry pointed to the inevitable relationship between mental deterioration and the harsh and punitive circumstances of detention.
This has been a hotly debated topic among medical professionals. Some doctors argue that we should not support a system of unacceptable standards that damages detainees and others point to the need to provide care and advocate for positive change.
Medical opinions overridden by government
In my view, the current situation on Manus is one of the most extreme forms of medical neglect ever countenanced by the Australian government and one where the consequences will have reverberations throughout broad health professions.
In practice, it appears that the Australian government remains adamant the clinicians are not the primary decision makers about the health needs of detainees and there have been serious outcomes where there are delays in treatment despite medical recommendations.
The case of the death of Hamid Khazaei from overwhelming sepsis (infection and multiple body system failure) in 2014 following repeated medical requests for transfer is one example of a system failing to provide care and the dismissal of medical expertise by officials.
It is events such as these, and the witnessing of mental deterioration and decline and self-harming and suicidal behaviour that causes significant moral distress to doctors.
Clinicians face core ethical dilemmas about their own ability to provide treatment within a system (offshore detention) which itself causes mental deterioration and psychological harm. Even the provision of treatment, such as with medication or psychological support, will have limited efficacy and is unlikely to provide a permanent solution.
Clinicians have a responsibility to document and alert government to abuses and to the impacts of harmful policy. This positive advocacy for voiceless and dis-empowered people is a fundamental tenant of medical practice.
Medical professionals are motivated by beliefs in the right to health care and view health as a human right. Advocacy is a fundamental part of this role and to have these principles dismissed or subjected to questioning for a particular political agenda – in this case that of immigration policy – is unacceptable.
Louise Newman is Director of the Centre for Women’s Mental Health at the Royal Women’s Hospital and Professor of Psychiatry, University of Melbourne
Disclosure: Louise Newman does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment
This article was originally published on The Conversation. Read the original article