An MBS review committee chairman has taken issue with reporting that says the changes do not reflect its findings.
The chair of the cardiac committee for the MBS review has defended changes that defund GP interpretation of ECGs and denied the government misled or misrepresented him and his colleagues.
The move has sparked outrage from doctors on social media and alarm from the AMA and RACGP, who are calling for the move to be scrapped or at least paused.
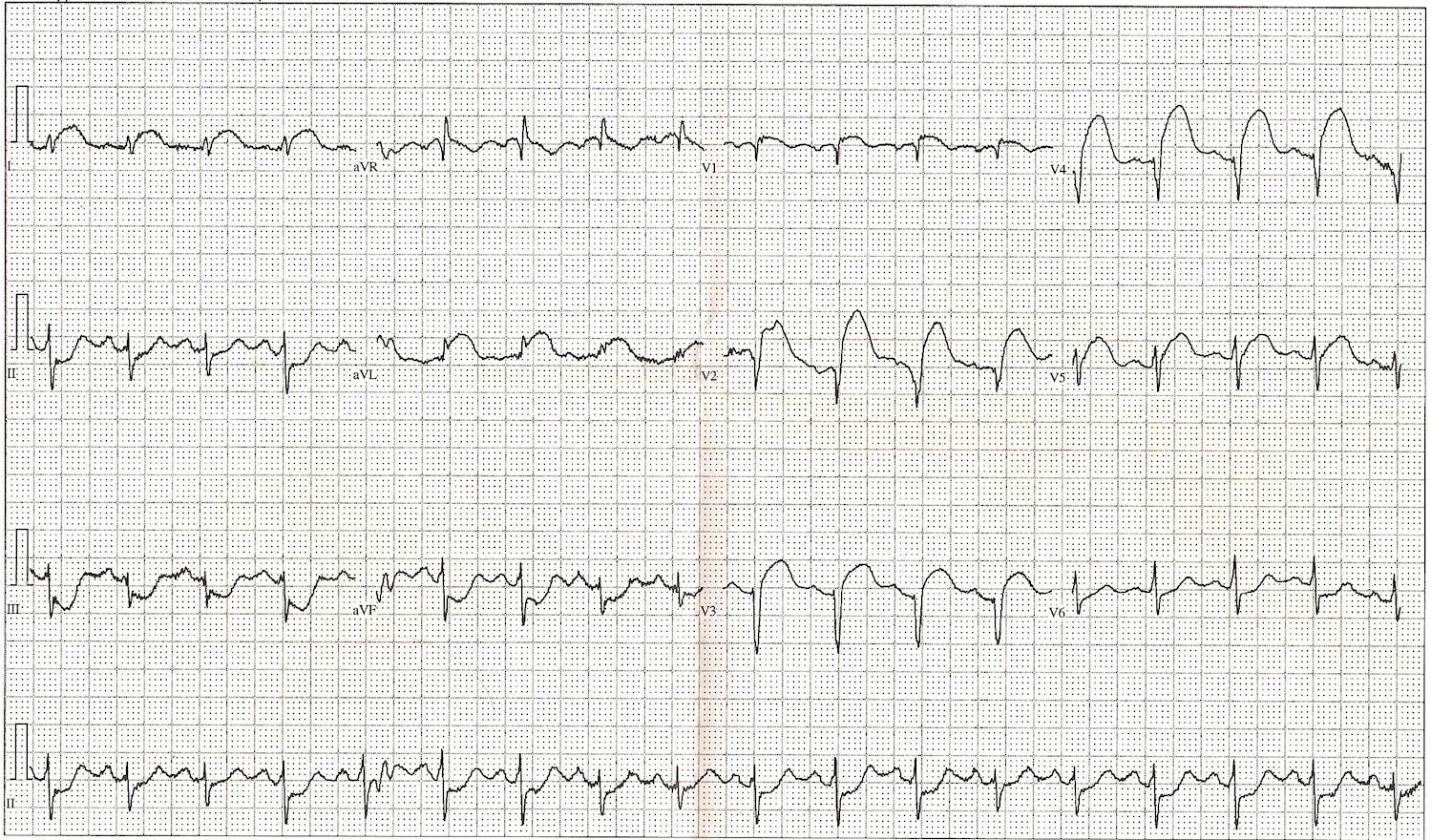
The changes are in response to 2018 recommendations from the MBS Review Taskforce, which raised concerns that “many ECGs are of low value” and that the service was growing at a rate of 7% per year – well above population growth.
As a result, Medicare has removed the ECG items 11700, 11701 and 11702 and created the new items 11704, 11705, 11707 and 11714.
Professor Richard Harper, chair of the Cardiac Services Clinical Committee of the MBS Review Taskforce, says that claims published in Australian Doctor that the government misrepresented him were incorrect.
The article, published on Tuesday, ran under the heading “‘Govt misrepresented us’: MBS review experts question ECG cuts”. It quoted Professor Harper and fellow committee member and GP Professor Mark Harris as saying the Department of Health’s move did not reflect the committee’s actual findings.
“The government has not misled myself, or my colleagues at any point in this process,” Professor Harper has since said in a statement.
It had in fact conducted a “lengthy, collaborative consultation” with clinical experts such as himself and representatives from CSANZ, the AMA and the RACGP.
“While this process has involved debate and compromise, the discussions were undertaken in good faith at all times.”
Professor Harper, emeritus director of Cardiology Monash Health and an adjunct professor of medicine at Monash University, said he had told Australian Doctor that he thought their views were being “misrepresented in the public discussion”.
“I am strongly of the belief these changes need to be made and will protect patient safety,” he added.
He made several arguments in favour of the MBS item number changes.
“Modern ECG machines used in general practice provide an automated report which experience has shown is generally very accurate,” he said. “The GP can check the automated report, provide his or her own interpretation as appropriate.”
GPs who were uncertain about the significance of the results could send it off to a cardiologist for assistance, he said.
Most patients would be receiving ECGs that did not pick up acute, life-threatening anomalies, he said. Those that did would need an immediate consultation with a cardiologist or to visit an emergency department.
“As Chair of the Clinical Committee I can assure all patients the committee undertook a rigorous assessment of these items in light of best clinical evidence and practice before making its recommendations,” he said, adding that the committee had provided no recommendations regarding fees.
Opposition health spokesman Chris Bowen said it “beggars belief that the government is cutting health care subsidies during a global health emergency”.
“GPs are qualified to interpret ECG tests, they should be endorsed for doing so, not defunded,” he said, adding that there were alternative mechanisms to curb overuse or unsafe use.
The RACGP and AMA called on the government to halt the changes, which will defund GP interpretation of ECGs, saying it will drive up prices and hospital visits for patients.
From August 1, GPs will no longer be eligible for MBS funding for reporting on 12-lead ECG traces, and instead will only be allowed to use item 11707 for tracing alone.
This will be reimbursed at $19.
The late RACGP president Dr Harry Nespolon said the college was “deeply disappointed” at the decision to reduce patient rebates for ECGs in general practice.
“These changes are likely to hurt patients through higher costs and inconvenience,” he said.
“The decision completely fails to recognise the work GPs do with ECGs – we perform interpretation, report results in patient records and determine actions that need to be taken, very often without needing to refer patients to another specialist for interpretation and reporting.”
He said the college had “advocated strongly against these changes for good reason”.
“Chronic conditions requiring ECGs and associated care like heart problems are increasing in Australia,” he said, adding that primary care was the most cost effective way of providing high-quality care for such patients.
“The government should be investing in primary care to keep patients out of the hospital system – instead we are seeing this ripped away.”
AMA president Dr Tony Bartone urged Health Minister Greg Hunt to halt the changes, in a letter obtained by TMR.
“The move to block GPs from access to what has been a commonly used MBS item or the proposed new item 11714 once again devalues the work that they do and potentially makes it harder for patients to access care,” Dr Bartone wrote.
“We are also concerned that GPs may simply refer patients, who they could otherwise quite easily treat, to their non-GP specialist colleagues.”
Dr Bartone said that the many GPs he had spoken to were “overwhelmingly critical” of the move, and that this new MBS rebate structure would make the mandated provision of ECG services uneconomic for many practices.
This change was made with little advance warning, triggering confusion and ire among GPs, many of whom took to social media to voice their displeasure.
“How can you defund the health sector during a global health crisis?” Newcastle GP Dr Kathleen Wild asked on Twitter.
“This is not low-value care. I do not think my patients would describe my immediate attention to their risk of arrhythmia and heart disease as low-value care.”
Geelong GP Dr Ern Chang issued an open letter to Health Minister Greg Hunt, saying the Sunday evening announcement of the changes came as a “rude and unexpected shock”.
All doctors were trained to perform and interpret ECGs, he wrote, and the test was “critical” for the day-to-day care of patients all around Australia, including those in rural and regional locations. Practices would now have to bill privately to pay for the expensive machines.
Other GPs said defunding the service would result in deskilling within general practice and unnecessary trips to the emergency department.
RACGP presidential nominee Dr Karen Price noted that while the move would save the federal government money, the costs would be pushed on to the states.