In this final part in our series on problem crying in babies, we look at evidence-based management of baby’s feeding, sleep and sensory needs and maternal mental health
FEEDS
EXAMINATION
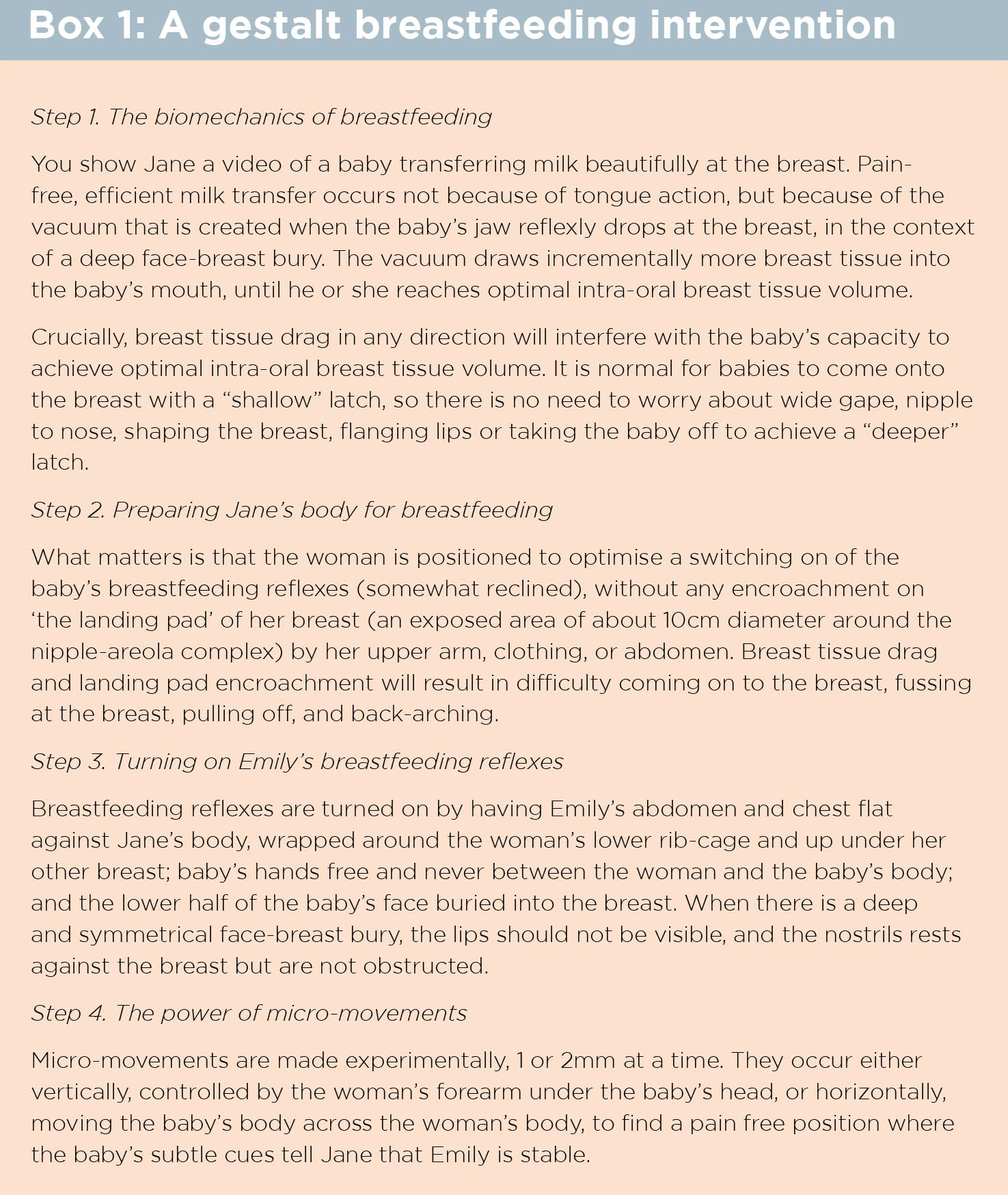
A brief observation of Jane and Emily breastfeeding demonstrates suboptimal fit and hold with significant positional instability and breast tissue drag, resulting in compromised milk transfer and fussiness at the breast. In addition, Emily shows behaviours consistent with conditioned dialling up at the breast.
MANAGEMENT
1. You explain that Emily’s fussing at the breast is not due to low supply, forceful letdown, or to swallowed air, reflux or gas pain. This means that Darren and Jane should avoid disrupting Emily by burping her or holding her upright during or after feeds.
2. You explain that breast tissue drag and positional instability are the cause of Emily’s difficulty in coming on to the breast, back-arching and pulling off while feeding.
3. You acknowledge how confusing this seems, because Jane has been regularly reassured that Emily’s “latch and positioning” are good. You explain you are using the gestalt approach to the biomechanics of breastfeeding, based on the latest ultrasound studies. You ask if Jane would be willing to try something different. With consent, you offer a focussed gestalt breastfeeding intervention, or refer to someone who can. (See Box 1) You also refer Jane to the Gestalt Breastfeeding Online Self-help Program.
4. You recommend implementing paced bottle-feeding, and direct Jane to a free demonstration video.
5. You explain that once the baby is positionally stable and transferring milk effectively, pumping is unnecessary: Emily becomes Jane’s best pump!
6. You explain that you think Emily has some conditioned dialling up, or sensitivity, at the breast, too. This is common, and comes about when the baby has a powerful drive to breastfeed, but things don’t work quite as well as everyone wanted. You explain you have strategies that usually help resolve this.
POOR SATIETY
Breastfed babies in Western countries cry more than their formula-fed counterparts, most likely due to widespread unidentified and unmanaged breastfeeding problems.2,3 A large WHO cohort show that breastfed babies gain 200-250gm a week in the first months of life.
Neuroprotective developmental care (NDC) proposes that babies cry due to satiety problems even when they are gaining weight at previously acceptable standards. 4 Marathon feeding and excessively frequent feeding are commonly signs of positional instability and suboptimal breastmilk transfer.
MANAGEMENT OF BOTH POOR SATIETY AND CONDITIONED DIALLING UP AT THE BREAST
You validate how incredibly upsetting it is when our babies don’t seem to want to breastfeed, and worse, when there are weight-gain worries, but you explain to Jane that it is very important Emily never feels under pressure to feed.
You invite Jane to grow positive experiences at the breast, and to minimise any negative experiences. You explain that many, if not most, women need to offer both breasts at least 12 times in a 24-hour period to maintain breastmilk supply, and to keep the baby dialled down and the days enjoyable. These feeds are likely to be highly variable in length and not always both breasts. Once underlying problems are sorted out, frequent flexible breastfeeds make the days easier, not harder.
You suggest that when Emily dials up at the breast, Jane focusses on responding with micro-movements and strategies for stabilising the fit and hold, but if this doesn’t help, that she stops the breastfeed and changes Emily’s sensory environment.
It’s important, though, that Jane feels free to offer the breast again within a short period of time. You recommend Jane uses the two tools of sensory nourishing and milk to get through the days, experimenting to see which will dial Emily down at any given time.
BABY’S SENSORY NEEDS
In the absence of supporting evidence, crying baby guidelines still commonly advise to avoid infant overstimulation, demonstrating interpretative bias. 5,6,7
The concept of overstimulation was first proposed by doctors in the early 1900s, concerned about the effects of modern trains, cars, and electric lighting on children’s nervous systems. 8 Yet the latest neuroscience, corroborated by evolutionary biology and cross-cultural studies, demonstrates that enriched sensory experience optimises developmental outcomes. 9 The NDC programs educate parents that infants may cry and fuss a lot due to a lack of rich and diverse sensory nourishment e.g. in the interiors of our homes.
Evidence does not support the belief that swaddling decreases crying and improves sleep, and since breastfeeding a baby while swaddled interferes with positional stability and should be avoided, re-swaddling after feeds unnecessarily rouses the baby. Similarly, the evidence shows that infant massage, 10 manipulative therapies, 11,12 and acupuncture do not decrease crying; since acupuncture is invasive, it should be avoided. 13,14
MANAGEMENT
Enquire if Jane and Darren have noticed that Emily dials down as soon as they step outside the front door. Explain that our babies are laying down neural templates for life in direct response to sensory input, and have a powerful biological drive for rich and changing sensory nourishment. Many babies cry a lot in the low sensory interior environments.
Suggest that Jane plans her days outside the home, to socialise, to attend activities and parent groups, to visit the shops, to visit the workplace, and to go for walks. Acknowledge that this advice seems scary when a woman has had breastfeeding problems, but you are working together to make breastfeeding much more dialled down.
Jane might want to set up outings to supportive friends and families homes at first. You explain that most primary carers feel initially daunted by this advice, but, in fact, life with the baby turns out to be so much easier out and about than when she stays at home.
Invite Jane to experiment with getting out of the house as much as she can for a week, then review and see what she thinks.
PARENT-BABY SLEEP
As my researcher heroes, Professor of Primary Care and GP Trisha Greenhalgh and Professor John Ioannidis, separately observe, authors’ interpretation and promotion of their research data is commonly biased by their desired goals. Moreover, the adoption of research by policy-makers and government institutions is commonly determined by the rhetoric of high-status individuals and organisations, not by the quality of evidence. 15,16
The current dominance of “sleep training” approaches to parent-baby sleep illustrates these problems.
THE COSTLY MERRY-GO-ROUND OF FIRST WAVE BEHAVIOURAL APPROACHES
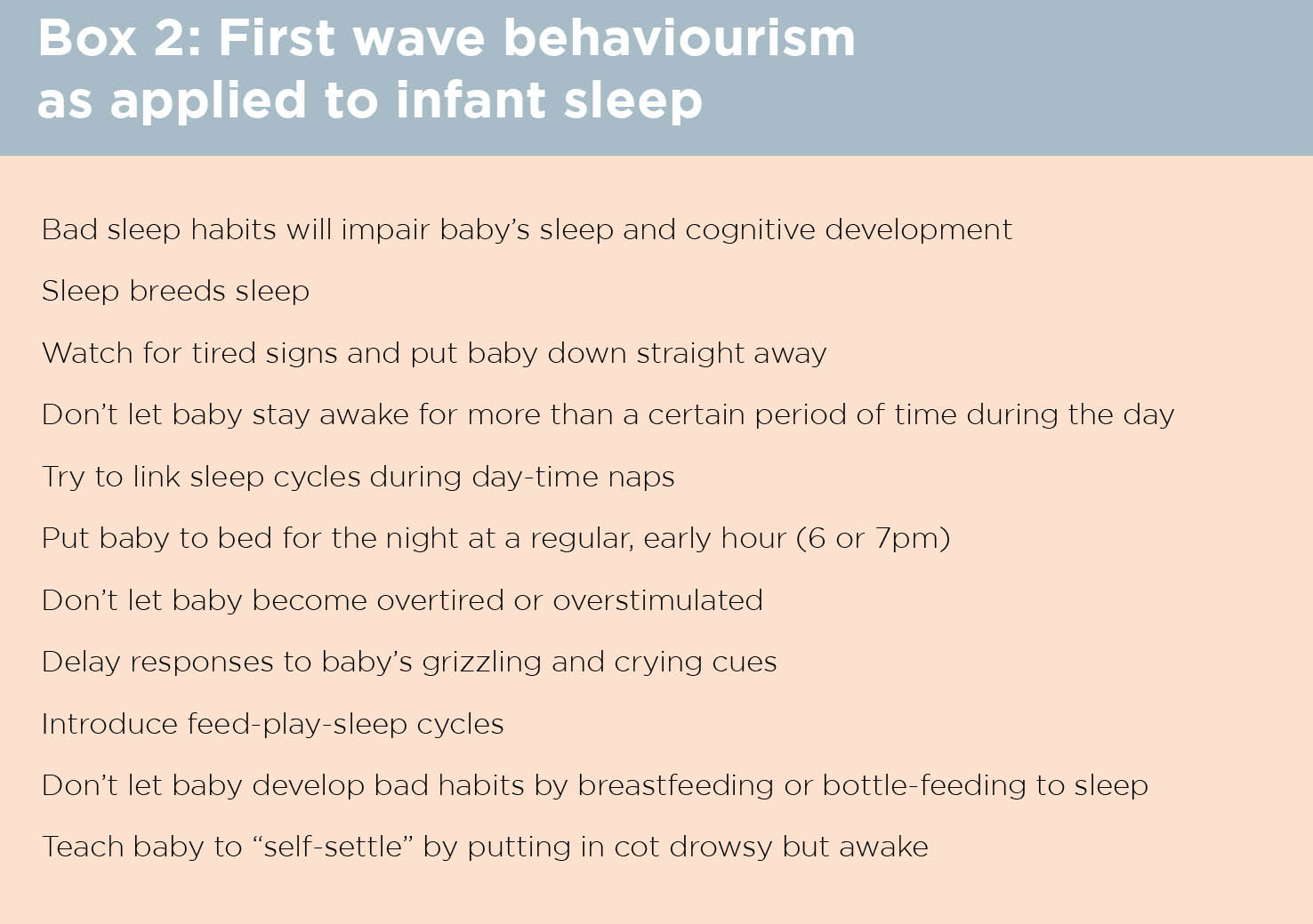
The school of psychology known as behaviourism arose in the 1950s and 1960s. It was soon applied to infant-care, also incorporating the pre-existing concept of overstimulation.
In Queensland high schools, this first wave of behaviourism (FWB) determined the strategies taught to girls like myself in our compulsory 1970s Mothercraft classes. (See Box 2)
Behaviourism has been extensively developed since then. The second wave of behaviourism acknowledged cognitions as interior behaviours, and gave rise to cognitive behavioural therapy, which has been well researched.
Most recently, a third wave of behaviourism acknowledges the context of behaviours, and has given rise to acceptance and commitment therapy, which has a rapidly growing evidence-base. Yet, remarkably, FWB continues as the dominant approach to parent-infant sleep in the English-speaking world.
FWB or “sleep training” approaches have been demonstrated to NOT decrease night-waking, NOT reliably improve maternal mood, NOT result in improved sleep or developmental outcomes in later childhood, and are associated with increased parental anxiety. 17-21
The known association between unsettled infant behaviour and behaviour problems in later childhood is cited as rationale to apply FWB as a public health strategy for infant sleep. 22 However, this association may in fact be mediated by the ubiquitous promotion of first wave behavioural approaches, either by health professionals, in parenting books, or social media, which exacerbate anxiety 21,23 and disrupt the infant’s circadian clock, worsening night-time sleep. 24-27
In an Australian example illustrating Professor Greenhalgh’s concerns about the power of research rhetoric, the program Baby Business was designed to prevent infant crying and sleep problems and associated postnatal depression symptoms, through the implementation of FWB strategies. 28
But a randomised controlled (RCT) trial of 781 families showed no improvement in crying or sleep problems. At four months, intervention parents had sort help from health professionals more often for their baby, and showed no improvement in depressive symptoms relative to controls. 29
In interpreting their data, however, the authors focus on a small, poorly defined subset of “frequent feeders”, subject to multiple unidentified confounders, though this subset finding is an irrelevance. 30
Baby Business continues to be promoted for helping parents manage their baby’s crying and sleep problems. The authors of two comparable large RCTs of FWB anticipatory guidance for infant sleep, in Canada and New Zealand, clearly state their findings of no impact on sleep. 31,32
As Professor Ioannidis’s team asks: what happens when a high profile “big idea” doesn’t work? They write that proponents tend to call for better design, more complex measures, and more research investment in the same approach.
But inability to prove efficacy in repeated trials signals that it is time to “sunset” the underperforming dominant idea and invest in innovative, “blue-sky” research, built from rigorous theoretical frames.33
Although proponents of FWB to infant sleep have called for better design, more complex measures, and more research investment when faced with systematic reviews demonstrating lack of effect, 34 it’s actually time to invest in innovation.
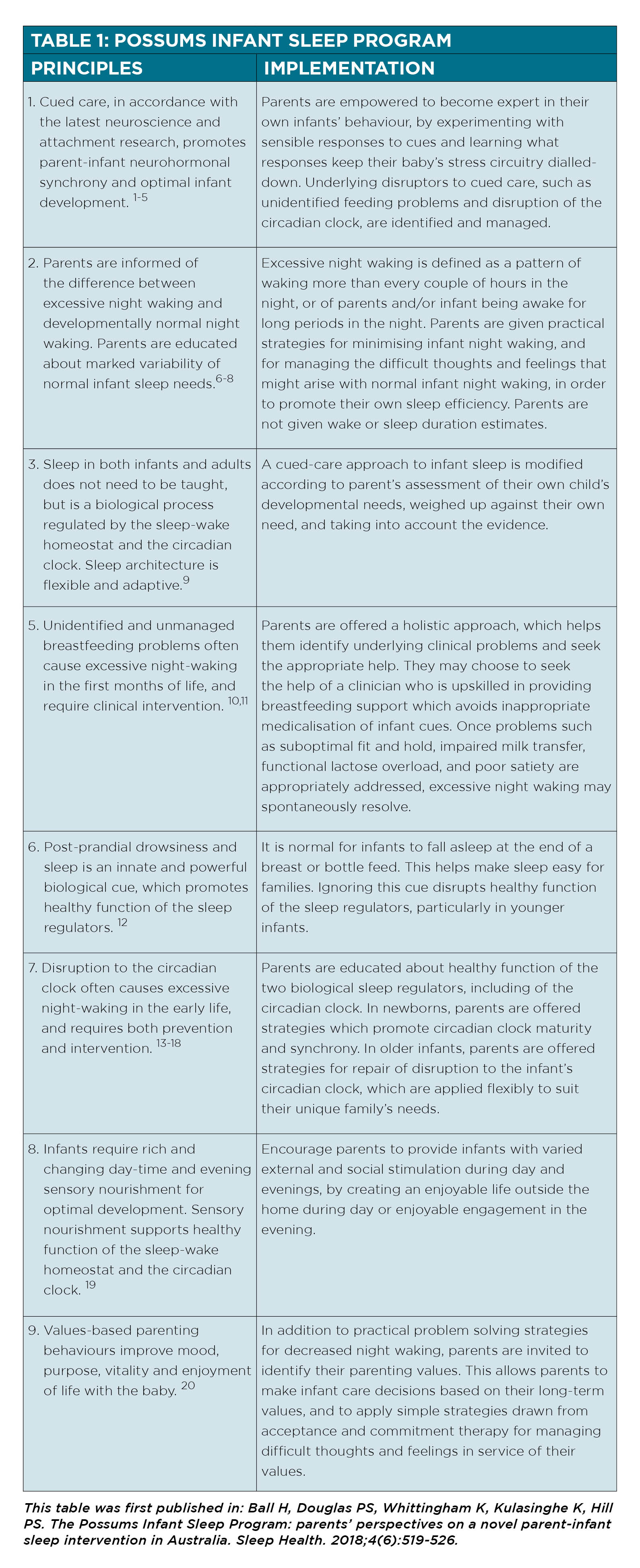
The Possums Sleep Program has a strong theoretical framework and has proven highly acceptable to Australian parents in preliminary evaluations, with improved sleep and quality of life outcomes. 35,36 (See Table 1) It has been adapted by the Durham University Parent-Infant Sleep Laboratory in the UK, who are trialling it in private and NHS settings.
The Possums Sleep Film is available as a self-help online program or can be licensed for health professional use in your clinic. 37
MANAGEMENT: POSSUMS SLEEP INTERVENTION
You explain to Jane and Darren that they do not need to try to make Emily sleep during the day, or to keep her asleep.
You suggest experimenting with richer sensory nourishment when she begins to dial up during the day, rather than thinking she needs to sleep.
Emily’s sleep regulators can be trusted to take the sleep she needs, in the context of satiety of milk and satiety of sensory nourishment.
The blocks of crying in the night indicate that Emily’s circadian clock has not yet matured, and that she is awake, not needing to sleep, but wanting sensory nourishment rather than in pain.
If Jane is having enjoyable days outside the home, meeting Emily’s sensory needs and not trying to put Emily to sleep, then Emily’s sleep looks after itself and will quickly consolidate at nights.
Maternal mental health (and not neglecting fathers’ or other carers’ mental health)
Crying baby guidelines commonly problematise or pathologise worried mothers, proposing that infant cry-fuss and sleep problems relate to maternal anxiety or vulnerable personalities who have difficulty limit-setting.
This is, I propose, a perpetuation of the 20th-century tendency to mother-blaming, now occurring in the context of health system failures which worsen parental anxiety.
Both cry-fuss problems and breastfeeding problems are critical modifiable risk factors for postnatal anxiety and depression. 38-41
High-level evidence concerning strategies for prevention and early intervention for perinatal mental health problems calls for clinical support for parenting skills (that is, to deal with the common problems of unsettled infant behaviour and breastfeeding difficulty), in order to optimise maternal mental health and associated infant developmental outcomes. 42-44
NDC integrates applied functional contextualism, a modern form of CBT popularly known as Acceptance and Commitment Therapy (ACT) into its programs.36, 45,46
NDC also includes a peer support program for parents, known as PIPPS.
MANAGEMENT
You explain that Jane’s elevated Edinburgh Depression Scale score shows how important it is now to take care her emotional well-being, and that you’d like to check in with her regularly for a little while. You direct Jane and Darren to a video that offers some simple ACT strategies which parents find useful as they manage the very difficult thoughts and feelings that arise when their baby is distressed.
When Jane sees you again in a week’s time, Emily is already significantly dialled down, fussing much less at the breast, and crying and fussing for no more than an hour a day overall. Jane has many questions, because the NDC approach is quite different to other advice she has received, and you carefully answer these. You observe a breastfeed and continue to consolidate the gestalt breastfeeding strategies.
In a third follow-up with Jane and Darren, a fortnight after the initial presentation, Emily is not crying much at all. Jane says she realises now she was tending to force the breastfeeds, because she felt she had to get in as much milk as possible in the allotted time.
Jane is enjoying her days socialising and walking outside the house, even though she is still tired.
Jane and Darren have also relaxed about Emily’s sleep. The evenings remain challenging, but between more frequent breastfeeding and Darren playing with Emily, bathing her, and taking her out for walks, they are managing better.
Emily wakes every two hours at night, but goes back to sleep quickly with a breastfeed. Jane is no longer pumping, and has stopped using formula. Emily is gaining 200gm/week. Jane’s EPDS is now nine. Jane and Darren say to you, with relief: “At last we are enjoying our baby.”
Dr Pamela Douglas is Medical Director, The Possums Centre, Greenslopes, Brisbane; Maternity Families and Newborn Centre, MHIQ Griffith University; Senior Lecturer, Discipline of General Practice, The University of Queensland; Author of The discontented little baby book: all you need to know about feeds, sleep and crying
www.possumsonline.com;
www.pameladouglas.com.au
References
1. Moore T, Arefadib N, Deery A, West S. The first thousand days: an evidence paper. Parkville, Victoria: Centre for Community Child Health, Murdoch Children’s Research Institute, 2017.
2. Wolke D, Bilgin A, Samara M. Systematic review and meta-analysis: fussing and crying durations and prevalence of colic in infants. Journal of Pedatrics. 2017;185:55-61.
3. de Lauzon-Guillain B, Wijndaele K, Clark M, Acerini CL, Hughes IA, Dunger DB, et al. Breastfeeding and infant temperament at age three months. PLoS ONE. 2012;7:e29326.
4. Huhtala V, Lehtonen L, Uvnas-Moberg K, Korvenranta H. Low plasma cholecystokinin levels in colicky infants. J Pediatr Gastroenterol Nutr. 2003;37:42-45.
5. Sung V. Infantile colic. Australian Prescriber. 2018;41(4):105-110.
6. Zeevenhooven J, Browne PD, L/Hoir MP, De Weerth C, Benninga MA. Infant colic: mechanisms and management. Nature Reviews: Gastroenterology and Hepatology. 2018;15:479-496.
7. Daelemans S, Peeters L, Hauser B, Vandenplas Y. Recent advances in understanding and managing infantile colic. F1000Research. 2018;1426:doi:10.12688/f11000research14940.12681.
8. Matricciani LA, Olds TS, Blunden SL, Rigney G, Williams MT. Never enough sleep: a brief history of sleep recommendations for children. Pediatrics. 2012;129:548.
9. Lickliter R. The integrated development of sensory organization. Clinics in Perinatology. 2011;38:591-603.
10. Bennett C, Underdown A, Barlow J. Massage for promoting mental and physical health in typically developing infants under the age of six months. Cochrane Database of Systematic Reviews. 2013;4:CD005038. doi: 005010.001002/14651858.CD14005038.pub14651853.
11. Posadzki P, Ernst E. Is spinal manipulation effective for paediatric conditions? An overview of systematic reviews. Focus on Alternative and Complementary Therapies. 2012;17:22-26.
12. Dobson D, Lucassen P, Miller J, Vlieger A, P P, G L. Manipulative therapies for infantile colic. Cochrane Database Syst Rev. 2012;12:Art. No.:CD004796.
13. Skjeie H, Skonnord T, Brekke M, Klovning A, Fetveit A, Landgren K, et al. Acupuncture treatments for infantile colic: a systematic review and individual patient data meta-analysis of blinding est validated randomised controlled trials. Scandinavian Journal of Primary Health Care. 2018;Jan 17:1-14.
14. Lee D, Lee H, Kim J, Kim T, Sung S, Leem J, et al. Acupuncture for infantile colic: a systematic review of randomised controlled trials. Evidence-Based Complementary and Alternative Medicine. 2018:doi: 10.1155/2018/7526234.
15. Ioannidis JPA. Evidence-based medicine has been hijacked: a report to David Sackett. Journal of Clinical Epidemiology. 2016:doi:org/10.1016/j.jclinepi.2016.1002.1012.
16. Greenhalgh T, Russell J. Reframing evidence synthesis as rhetorical action in the policy making drama. Healthcare Policy. 2005;1:31-39.
17. Kempler L, Sharpe L, Miller CB, Bartlett DJ. Do psychosocial sleep interventions improve infant sleep or maternal mood in the postnatal period? A systematic review and meta-analysis of randomised controlled trials. Sleep Medicine Reviews. 2016;29:15-22.
18. Douglas P, Hill PS. Behavioural sleep interventions in the first six months of life do not improve outcomes for mothers or infants: a systematic review. J Dev Behav Pediatr. 2013;34:497–507.
19. Bryanton J, Beck C, Montelpare W. Postnatal parental education for optimizing infant general health and parent-infant relationships. Cochrane Database Syst Rev. 2013(11):CD004068. DOI: 004010.001002/14651858.CD14004068.pub14651854.
20. NHMRC report on the evidence: promoting social and emotional development and wellbeing of infants in pregnancy and the first year of life. http://www.nhmrc.gov.au: Australian Government, 2017.
21. Etherton H, Blunden S, Hauck Y. Discussion of extinction-based behavioral sleep interventions for young children and reasons why parents may find them difficult. Journal of Clinical Sleep Medicine. 2016;12(11):1535-1543.
22. Williams KE, Berthelsen D, Walker S, Nicholson JM. A Developmental Cascade Model of Behavioral Sleep Problems and Emotional and Attentional Self-Regulation Across Early Childhood. Behav Sleep Med. 2017;15(1):1-21.
23. Blunden S, Etherton H, Hauck Y. Resistance to Cry Intensive Sleep Intervention in Young Children: Are We Ignoring Children’s Cries or Parental Concerns? Children. 2016;3(2):8.
24. Appleman K, Figueiro M, Rea M. Controlling light-dark exposure patterns rather than sleep schedules determines circadian phase. Sleep Medicine. 2013: DOI:10.1016/j.sleep.2012.1012.1011
25. Thomas KA, Burr RL, Spieker S, Lee J, Chen J. Mother-infant circadian rhythm: development of individual patterns and dyadic synchrony. Early Human Development. 2014;90(12):885-890.
26. Gallaher KGH, Slyepchenko A, Frey BN, Urstad K, Dorheim SK. The role of circadian rhythms in postpartum sleep and mood. Sleep Medicine Clinics. 2018;13(3):359-374.
27. Morales-Munoz I, Partonen T, Saarenpaa-Heikkila O, Kylliainen A, Polkki P, Porkka-Heiskanen T, et al. The role of parental circadian preference in the onset of sleep difficulties in early childhood. Sleep Medicine. 2018;54:223-230.
28. Cook F, Bayer J, Le HN, Mensah F, Cann W, Hiscock H. Baby Business: a randomised controlled trial of a universal parenting program that aims to prevent early infant sleep and cry problems and associated parental depression. BMC Pediatr. 2012;12:13.
29. Hiscock H, Cook F, Bayer J, Le HN, Mensah F, Cann W, et al. Preventing early infant sleep and crying problems and postnatal depression: a randomized trial. Pediatrics. 2014;133:1-9.
30. Douglas PS, Whittingham K. Response to ‘Sleeping like a baby? Infant sleep impact on care givers and current controversies’. Journal of Paediatrics and Child Health. 2015;51:234.
31. Stremler R, Hodnett E, Kenton L, Lee K, Weiss S, Weston J, et al. Effect of behavioural-educational intervention on sleep for primiparous women and their infants in early postpartum: multisite randomised controlled trial. BMJ. 2013;346:doi: 10.1136/bmj.f1164.
32. Galland BC, Sayers RM, Cameron SL, Gray AR, Heath AM, Lawrence JA, et al. Anticipatory guidance to prevent infant sleep problems within a randomised controlled trial: infant, maternal and partner outcomes at 6 months of age. BMJ Open. 2017;7(5).
33. Joyner MJ, Paneth N, Ioannidis JPA. What happens when underperforming big ideas in research become entrenched? JAMA. 2016;316(13):Volume 316, Number 313.
34. Sadeh A, Mindell J. Infant sleep interventions – methodological and conceptual issues. Sleep Medicine Reviews. 2016;2016:123-125.
35. Ball H, Douglas PS, Whittingham K, Kulasinghe K, Hill PS. The Possums Infant Sleep Program: parents’ perspectives on a novel parent-infant sleep intervention in Australia. Sleep Health. 2018;4(6):519-526.
36. Whittingham K, Douglas PS. Optimising parent-infant sleep from birth to 6 months: a new paradigm. Infant Mental Health Journal. 2014;35:614-623.
37. Douglas PS. The Possums Sleep Program: supporting easy, healthy parent-infant sleep. International Journal of Birth and Parent Education. 2018;6(1):13-16.
38. Vik T, Grote V, Escribano J, Socha J, Verduci E, Fritsch M, et al. Infantile colic, prolonged crying and maternal postnatal depression. Acta Paediatr. 2009;8:1344-1348.
39. Dias CC, Figueiredo B. Breastfeeding and depression: a systematic review of the literature. Journal of Affective Disorders. 2015;171:142-154.
40. Fallon V, Groves R, Halford JC, Bennett KM, Harrold JA. Postpartum Anxiety and Infant-Feeding Outcomes: A Systematic Review. J Hum Lact. 2016.
41. Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104(467):96-113.
42. Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384:1800-1819.
43. Tsivos ZL, Calam R, Sanders MR, Wittkowski A. Interventions for postnatal depression assessing the mother-infant relationship and child develomental outcomes: a systematic review. International Journal of Women’s Health. 2015;23:429-447.
44. Werner EA, Miller M, Osborne L, Kuzava S, Monk C. Preventing postpartum depression: review and recommendations. Archives of Womens Mental Health. 2015;18(1):41-60.
45. Whittingham K, Douglas PS. “Possums”: building contextual behavioural science into an innovative evidence-based approach to parenting support in early life. In: Kirkaldy B, editor. Psychotherapy in parenthood and beyond. Turin, Italy: Edizioni Minerva Medica; 2016. p. 43-56.
46. Douglas PS, Keogh R. Gestalt breastfeeding: helping mothers and infants optimise positional stability and intra-oral breast tissue volume for effective, pain-free milk transfer. Journal of Human Lactation. 2017;33(3):509–518.
Table references
1. Evans CA, L PC. The emergence of mother-infant co-regulation during the first year: links to infants’ developmental status and attachment. Infant behavior and development. 2009;2009:147-158.
2.Swain JE, Konrath S, Dayton CJ, Finegood ED. Toward a neuroscience of interactive parent-infant dyad empathy. Behavioral and brain sciences. 2013;36:438-439.
3.Winberg J. Mother and newborn baby: mutual regulation of physiology and behavior – a selective review. Dev Psychobiol. 2005;47(217-229):217-229.
4.Swain JE. Becoming a parent – biobehavioral and brain science perspectives. Curr Probl Pediatr Adolesc Health Care. 2011;41(7):192-196.
5. Leclere C, Viaux S, Avril M, Achard C, Chetouani M, Missonnier S, et al. Why synchrony matters during mother-child interactions: a systematic review. Plos One. 2014;9(12):e113571.
6. Galland BC, Taylor BJ, Elder DE, Herbison P. Normal sleep patterns in infants and children: a systematic review of observational studies. Sleep Medicine Reviews. 2012;16:213-222.
7. Dias CC, Figueriedo B, Rocha M, Field T. Reference values and changes in infant sleep-wake behaviour during the first 12 months of life: a systematic review. Journal of Sleep Research. 2018:doi:10.111/jsr.12654.
8. Pennestri M-H, Laganiere C, Bouvette-Turcot A-A, Pokhvisneva I, Steiner M, Jeaney MJ, et al. Uninterrupted infant sleep, development, and maternal mood. Pediatrics. 2018;142(6):e20174330.
9. Jenni OG, Carskadon MA. Sleep behavior and sleep regulation from infancy through adolescence: normative aspects. Sleep Medicine Clinics. 2007;2(321-329).
10. Douglas PS, Geddes DB. Practice-based interpretation of ultrasound studies leads the way to less pharmaceutical and surgical intervention for breastfeeding babies and more effective clinical support. Midwifery. 2018;58:145–155.
11. Douglas PS, Hill PS. A neurobiological model for cry-fuss problems in the first three to four months of life. Med Hypotheses. 2013;81:816-822.
12. Maehara K, Mori E, Iwata H, Sakajo A, Aoki K, Morita A. Postpartum maternal function and parenting stress: comparison by feeding methods. International Journal of Nursing Practice. 2017;Suppl 1:doi:10.111/ijn.12549.
13. Thorpe K, Staton S, Sawyer E, Pattinson C, Haden C, Smith S. Napping, development and health from 0 to 5 years: a systematic review. BMJ. 2015;100:615-622.
14. Thomas KA, Burr RL, Spieker S, Lee J, Chen J. Mother-infant circadian rhythm: development of individual patterns and dyadic synchrony. Early Human Development. 2014;90(12):885-890.
15. Akacem LD, Simpkin CT, Carskadon MA, Wright KP, Jenni OG, Achermann P, et al. The timing of the circadian clock and sleep differ between napping and non-napping toddlers. Plos One. 2015;10(4):e0125181.
16. Lillis TA, Hamilton NA, Pressman SD, Khou CS. The association of daytme maternal napping and exercise with nighttime sleep in first-time mothers between 3 and 6 months postpartum. Behav Sleep Med. 2016:doi:10.1080/15402002.15402016.11239580.
17. Gallaher KGH, Slyepchenko A, Frey BN, Urstad K, Dorheim SK. The role of circadian rhythms in postpartum sleep and mood. Sleep Medicine Clinics. 2018;13(3):359-374.
18. Morales-Munoz I, Partonen T, Saarenpaa-Heikkila O, Kylliainen A, Polkki P, Porkka-Heiskanen T, et al. The role of parental circadian preference in the onset of sleep difficulties in early childhood. Sleep Medicine. 2018;54:223-230.
19. Lickliter R. The integrated development of sensory organization. Clinics in Perinatology. 2011;38:591-603.
20. Whittingham K, Douglas PS. “Possums”: building contextual behavioural science into an innovative evidence-based approach to parenting support in early life. In: Kirkaldy B, editor. Psychotherapy in parenthood and beyond. Turin, Italy: Edizioni Minerva Medica; 2016. p. 43-56.