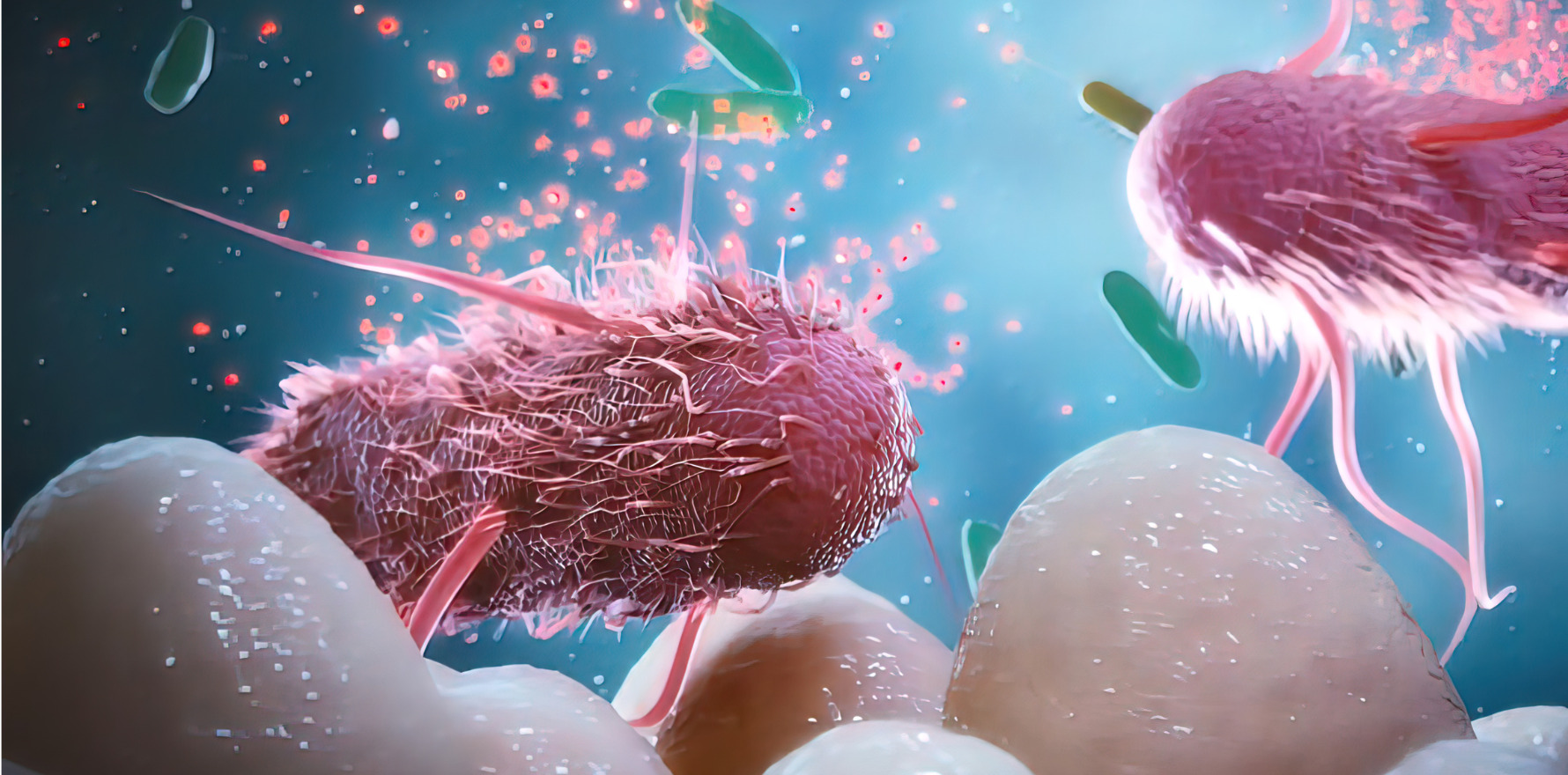
New research backs the theory that bacteria may play a causal role in the development of this rheumatological condition.
As an Australian trial of a novel live biotherapeutic kicks off, new evidence has added weight to the suggestion that Prevotella copri bacteria may have a causative role in rheumatoid arthritis
Research in Arthritis & Rheumatology reported an abnormal immune response to a Prevotella copri protein, Pc-p27, in patients at various stages of the disease. While previously observed in other studies of patients with established RA, the current study also looked at people with pre-clinical and early RA.
The American study, led by University of Colorado researcher Jennifer Seifert, looked at 98 control-matched pairs of people with rheumatoid arthritis and an additional 67 control-matched pairs of people who were at risk of developing the disease.
They found that people who were either at risk of developing RA or had early RA had numerically higher levels of IgG Pc-p27 antibodies than non-RA controls, though the differences were not statistically significant. Patients at later stages of the disease had significantly increased levels of IgA Pc-p27antibodies compared with non-RA matched controls.
Limitations of the study include the small numbers, precluding analyses of subsets of people with RA (for example, RF+ vs RF-), and the reliance on only one P. copri protein, Pc-p27.
In terms of mechanism, which the authors acknowledged was “not yet well understood”, they hypothesised that “certain Prevotella spp., especially Pc, may bind to the gut mucosa and periodically escape into the systemic circulation where they stimulate systemic immune responses”.
“Moreover, these organisms or their components may sometimes reach joints, perhaps within cells, where they may shape or amplify immune responses.”
Meanwhile, Australian researchers are conducting a clinical trial measuring whether introducing Lactobacillus species compounds, made by biopharmaceutical company Servatus, could be associated with a reduction in RA symptoms.
Queensland rheumatologist Professor Peter Nash, who is leading the trial, said there was a scientific basis for efficacy and that, if successful, the findings could help fill a “huge unmet need”.
“There’s a lot of interest in the microbiome, not just in rheumatoid arthritis but particularly in the spondyloarthropathies as well, either as a causative factor or an amplifying factor or a driving factor or a resistance to treatment factor,” he told Rheumatology Republic.
“A recent article I saw suggested that what bugs you’ve got in your gut can make you more or less responsive to the standard therapies that we use, such as methotrexate.”
In an animal model, Lactobacillus was roughly as effective as a JAK inhibitor, he said. If successful, Lactobacillus compounds could potentially replace anti-inflammatories in RA treatment.
“People are very interested in whether changing the microbiome can help treat the disease or even just ameliorate symptoms,” Professor Nash said.
“And patients are very keen to find a diet cure for improvement of their arthritis.”
- Professor Nash’s team is currently recruiting RA patients on methotrexate for the Lactobacillus trial. See the trial’s website for more information.