Japan has banned screaming on rollercoasters in an attempt to reduce the risk of COVID-19 transmission.
Welcome to The Medical Republic‘s COVID Catch-Up.
It’s the day’s COVID-19 news into one convenient post. Got any tips, comments or feedback? Email me at bianca@biancanogrady.com.
9 July
- Japanese rollercoasters ban screaming to reduce COVID-19 transmission risk.
- Male, older age, non-white ethnicity and deprivation all associated with greater COVID-19 mortality.
- All-cause mortality in hospitalised COVID-19 patients at around 10%, study suggests.
- COVID-19 infection rate in US prisons more than five times that of general population.
- Victorian healthcare facilities and hospitals mandate face-masks for patients, staff and visitors.
- On Japanese rollercoasters, no one can hear you scream. At least, that’s the hope, as Japan apparently bans screaming on its newly-reopened thrill rides in an attempt to reduce the risk of COVID-19 transmission among passengers, according to a report in The Wall Street Journal.
- The largest cohort study yet in COVID-19 patients has found being male, older, non-white, living with greater deprivation, and comorbidities such as diabetes and severe asthma are all significantly associated with greater COVID-19 mortality.
The study, published in Nature, analysed data from 10,926 COVID-19-related deaths in a population of more than 17 million adults in the United Kingdom. Researchers saw that individuals aged 80 years or older had a 20-times higher odds of COVID-19 mortality than those aged 50-59 years, while males had a 59% higher odds of mortality than females.
Patients experiencing the greatest levels of deprivation had an 80% higher mortality than those who experienced the least deprivation, and this was not explained by pre-existing conditions or clinical risk factors.
All non-white ethnicities were also associated with increased mortality, and the authors noted that this was evident even after adjusting for the higher prevalence of comorbidities and deprivation.
“Subsequent studies are needed to investigate the interplay of additional factors we were unable to explore, including employment, access to personal protective equipment and related risk of exposure to infection and household density,” the authors wrote. - Around one in ten in adults admitted to hospital with COVID-19 will die, according to a systematic review and meta-analysis of 44 studies that the authors warned consist of very low quality evidence.
The paper, published in Critical Care, looked at the association between acute complications of COVID-19 and mortality in studies from Asia, Europe and the Americas involving a total of 14,866 patients hospitalised with laboratory-confirmed COVID-19.
This suggested an all-cause mortality rate of 10%. Among patients who were admitted to intensive care, the mortality rate was 34%, among those needing invasive mechanical ventilation it was 83%, and among patients who developed acute respiratory distress syndrome, the mortality rate was 75%.
However the authors stressed that the studies were all of very low quality because of heterogeneity of patient populations, and the risk of bias. - The case rate for COVID-19 infections in US prisons is more than five times that of the general population, according to a paper in JAMA.
Analysis of data collected by the UCLA Law COVID-19 Behind Bars Data Project of more than 42,000 cases of COVID-19 in prisoners between March 31 to June 6, revealed a case rate of 3251 per 100,000 prisoners, compared to a care rate of 587 per 100,000 for the general US population. The crude death rate in prisons was also higher – 39 deaths per 100,000 compared to 29 deaths per 100,000 in the general population. However, after accounting for the lower proportion of the prison population that are aged 65 years or older – a higher risk age group for COVID-19 mortality – the adjusted death rate in prisons was three times higher than in the general population. - Four patients and a staff member have tested positive for COVID-19 at Brunswick Private Hospital in Melbourne, and five new cases have been linked to five different aged care facilities or services; Doutta Galla, Glendale Aged Care, Uniting AgeWell, BaptCare Karana and Mercy Health. Several Victorian health facilities, including Royal Melbourne Hospital, Western Health and all Cabrini-operated facilities now require all staff, patients and visitors to wear face masks.
Stage three restrictions are now in force across metropolitan Melbourne and Mitchell Shire. Residents can only leave their homes to shop for food and essential items; for care and caregiving; for daily exercise; or for work and study that cannot be done at home.
The three new cases reported in the ACT yesterday have been confirmed as three people in their twenties, two of whom returned from a Victorian hotspot last Thursday and the third is a household contact of those two cases.
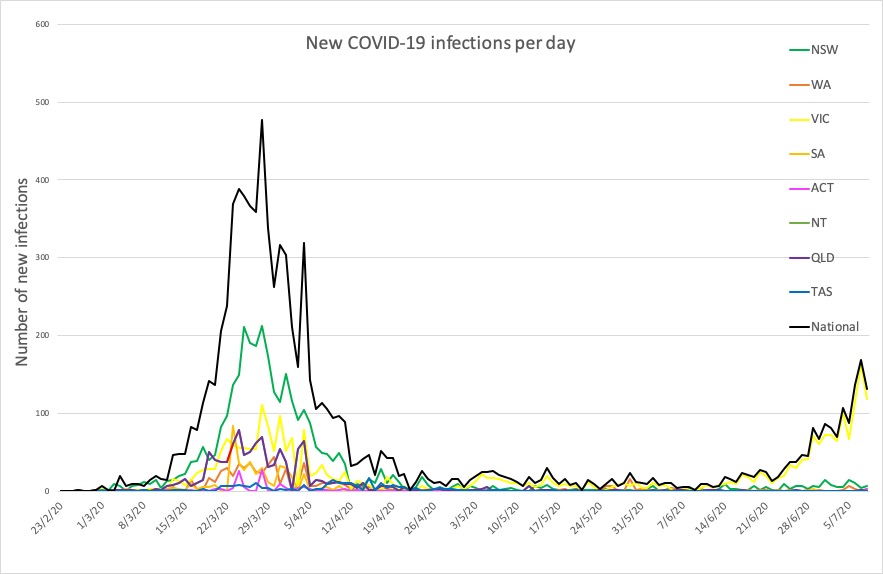
Here are the latest confirmed COVID-19 infection figures around Australia, to 9pm Wednesday:
National – 8886, with 106 deaths and 7487 recovered
ACT – 111
NSW – 2440
NT – 30
QLD – 1068
SA – 443
TAS – 228
VIC – 2942
WA – 624