Psychiatric morbidity may be part of the prodromal phase of this neurological condition.
People with multiple sclerosis are almost twice as likely to experience mental illness in the five years preceding their diagnosis, making it a possible early warning sign for the disease.
Psychiatric comorbidities are more common among people with the condition, but less is known about their prevalence in the lead up to their diagnosis.
“For a long time, it was thought that MS only really began clinically when a person experienced their first demyelinating event, such as in the form of vision problems. But we’ve come to understand there is a whole period preceding those events where the disease presents itself in more indirect ways,” study author, epidemiologist Professor Helen Tremlett, told media.
Professor Tremlett and colleagues analysed British Columbian database information on MS patients and healthy peers to identify two cohorts of MS patients: an administrative cohort (patients with three or more MS-specific hospital, physician or prescription diagnostic or drug codes) and a clinical cohort (patients diagnosed in one of the provinces’ four MS clinics). Each patient in both cohorts was matched with up to five healthy controls for comparison.
Twenty-eight percent of the MS patients in the administrative cohort had a psychiatric morbidity in the five years before their first MS-related claim, compared to 15% of those with no record of MS.
Similarly, 22% of MS patients in the clinical cohort had a psychiatric comorbidity in the five years before their diagnosis was made, compared to 14% of the healthy group.
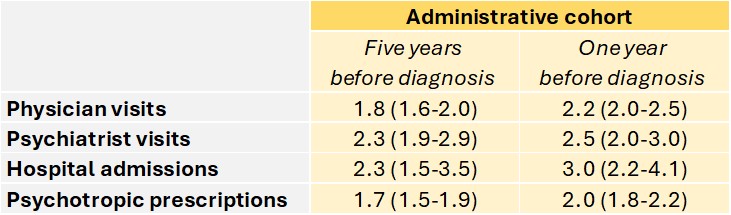
The database analysis showed MS patients in the administrative cohort had a higher rate of physician visits for a psychiatric morbidity, psychiatrist visits, psychiatric-related hospital admissions and psychotropic medication prescriptions in the five years before their first MS-related claim compared to controls, after adjusting for age, sex, socioeconomic status, and year of MS-related claim.
“While we’re not suggesting that these conditions alone can be a predictor of MS, they may be one piece of the MS prodrome puzzle and a potential signal when combined with other factors,” said neurologist and study author Associate Professor Anibal Chertcoff.
Common underlying mechanisms (such as low-grade inflammation), risk factors (obesity, adverse childhood events) and genetic determinants could contribute to the development of MS and psychiatric comorbidities, the researchers said.
The authors of an accompanying editorial acknowledged the “undoubtable” burden of psychiatric symptoms prior and during MS but stressed the need to remember that not every patient with a psychiatric condition will go on to develop MS.
“Considering how high the prevalence of psychiatric morbidity is in the general population, it is not feasible to refer every patient with psychiatric symptoms to a neurologist,” they wrote.


